5.2 The Respiratory System
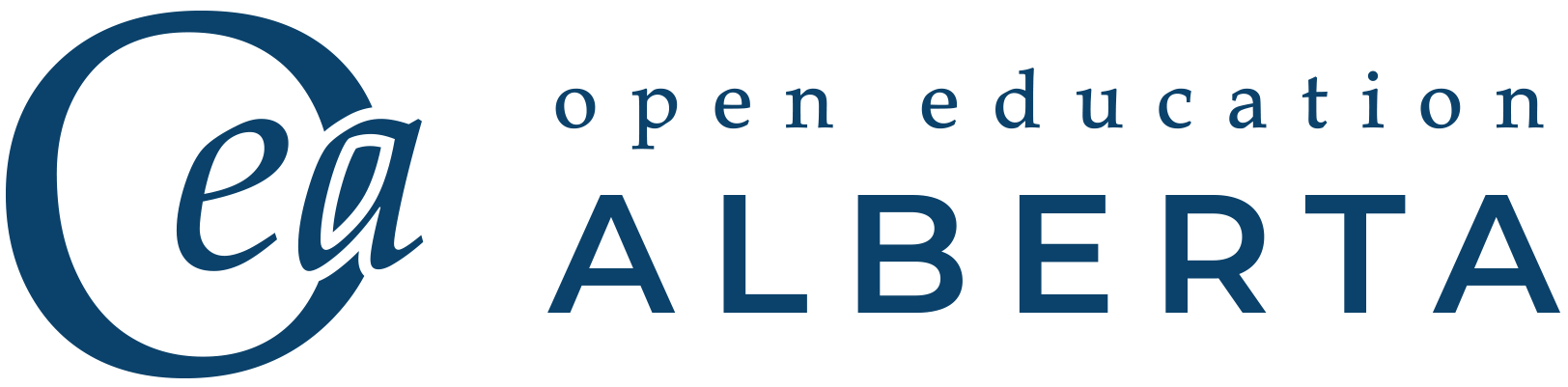
The major organs of the respiratory system function primarily to provide oxygen to body tissues for cellular respiration, remove the waste product carbon dioxide, and help maintain the acid-base balance. Portions of the respiratory system are also used for non-vital functions such as sensing odours, speech production, and straining, such as during childbirth or coughing. These components, as well as an overview of the whole respiratory system, are show in Fig. 5.1.
Functionally, the respiratory system can be divided into a conducting zone and a respiratory zone. The conducting zone includes the organs and structures not directly involved in gas exchange. Gas exchange occurs in the respiratory zone.
Conducting Zone Components
Nose
The major entrance and exit for the respiratory system is through the nose. Several bones help form the walls of the nasal cavity and create air-containing spaces called the paranasal sinuses, which serve to warm and humidify incoming air. These sinuses are lined with mucosa. Each paranasal sinus is named for its associated bone: frontal sinus, maxillary sinus, sphenoidal sinus, and ethmoidal sinus. The sinuses produce mucus and lighten the weight of the skull.
The nostrils, also called the nares, and the anterior portion of the nasal cavities are lined with mucous membranes and contain sebaceous glands and hair follicles that prevent the passage of large debris, such as dirt, through the nasal cavity. An olfactory epithelium that detects odours is located deeper in the nasal cavity.
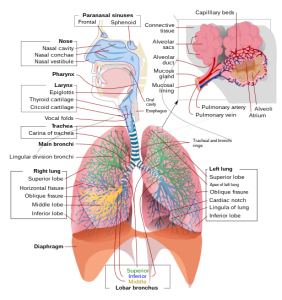
Pharynx
The pharynx is a tube formed by skeletal muscle and lined with mucous membrane that is continuous with that of the nasal cavity. The pharynx is divided into three major regions: the nasopharynx, oropharynx, and laryngopharynx (Fig. 5.2).
The nasopharynx serves as an airway passage to the rest of the respiratory system. At the top of the nasopharynx are the pharyngeal tonsils. Also called adenoids, the pharyngeal tonsils are an aggregate of lymphoid reticular tissue similar to lymph nodes and lie at the superior portion of the nasopharynx. The function of the pharyngeal tonsils is not well understood, but they contain a rich supply of lymphocytes and are covered with ciliated epithelium that traps and destroys invading pathogens that enter during inhalation. The pharyngeal tonsils are large in children, but interestingly, they tend to regress with age and may even disappear. The uvula is a small, bulbous, teardrop-shaped structure located at the apex of the soft palate. Both the uvula and soft palate move like a pendulum during swallowing, swinging upward to close off the nasopharynx to prevent ingested materials from entering the nasal cavity. In addition, auditory tubes that connect to each middle ear cavity open into the nasopharynx. This connection is why colds often lead to ear infections.
The oropharynx is a passageway for both air and food. It is bordered superiorly by the nasopharynx and anteriorly by the oral cavity. The oropharynx contains two distinct sets of tonsils—the palatine and lingual tonsils. The palatine tonsils are a pair of structures located laterally in the oropharynx. The lingual tonsils are located at the base of the tongue. Similar to the pharyngeal tonsils, the palatine and lingual tonsils are composed of lymphoid tissue and trap and destroy pathogens entering the body through the oral or nasal cavities.
The laryngopharynx is inferior to the oropharynx and posterior to the larynx. It continues the route for ingested material and air until its inferior end, where the digestive and respiratory systems diverge. Anteriorly, the laryngopharynx opens into the larynx, whereas posteriorly, it enters the esophagus.
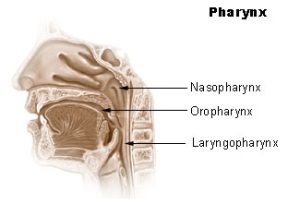
Larynx
The larynx is a cartilaginous structure inferior to the laryngopharynx that connects the pharynx to the trachea and helps regulate the volume of air that enters and leaves the lungs. The larynx is formed by several pieces of cartilage. Three large cartilage pieces—the thyroid cartilage (anterior), epiglottis (superior), and cricoid cartilage (inferior)—form the major structure of the larynx. The thyroid cartilage is the largest piece of cartilage and consists of the laryngeal prominence, or “Adam’s apple,” which tends to be more prominent in males. The thick cricoid cartilage forms a ring with a wide posterior region and a thinner anterior region. Three smaller, paired cartilages—the arytenoids, corniculates, and cuneiforms—attach to the epiglottis and the vocal cords and muscles that help move the vocal cords to produce speech.
The epiglottis, attached to the thyroid cartilage, is a very flexible piece of elastic cartilage that covers the opening of the trachea (Fig. 5.3). When in the “closed” position, the unattached end of the epiglottis rests on the glottis. The act of swallowing causes the pharynx and larynx to lift upward, allowing the pharynx to expand and the epiglottis of the larynx to swing downward, closing the opening to the trachea. These movements produce a larger area for food to pass through while preventing food and beverages from entering the trachea.
Trachea
The trachea (windpipe) extends from the larynx towards the lungs (Fig. 5.4). The trachea is formed by 16 to 20 stacked, C-shaped pieces of hyaline cartilage that are joined by dense connective tissue. The trachealis muscle and elastic connective tissue together form the fibroelastic membrane, a flexible membrane that closes the posterior surface of the trachea, connecting the C-shaped cartilages. The fibroelastic membrane allows the trachea to stretch and expand slightly during inhalation and exhalation, while the rings of cartilage provide structural support and prevent the trachea from collapsing. In addition, the trachealis muscle can contract to force air through the trachea during exhalation. The trachea is lined with pseudostratified ciliated columnar epithelium, which is continuous with the larynx. The esophagus borders the trachea posteriorly.
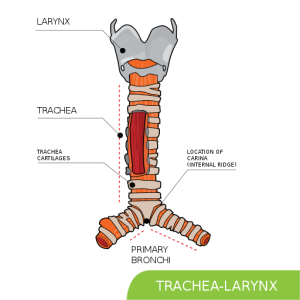
Bronchial Tree
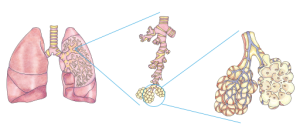
The trachea branches into the right and left primary bronchi. These bronchi are also lined by pseudostratified ciliated columnar epithelium containing mucus-producing goblet cells. Rings of cartilage, similar to those of the trachea, support the structure of the bronchi and prevent them from collapsing. The primary bronchi enter the lungs at the hilum, a concave region where blood vessels, lymphatic vessels, and nerves also enter the lungs. The bronchi continue to branch into a bronchial tree. Bronchial tree (or respiratory tree) is the collective term used for these multiple-branched bronchi. The main function of the bronchi, like other conducting zone structures, is to provide a passageway for air to move into and out of the lungs. In addition, the mucous membrane traps debris and pathogens.
Bronchioles branch from the tertiary bronchi. About 1 mm in diameter, they further branch until they become the tiny terminal bronchioles, which lead to the structures of gas exchange. There are more than 1,000 terminal bronchioles in each lung. The muscular walls of the bronchioles do not contain cartilage like those of the bronchi, but they can change the size of the tubing to increase or decrease airflow through the tube see Fig. 5.5.
Respiratory Zone Components
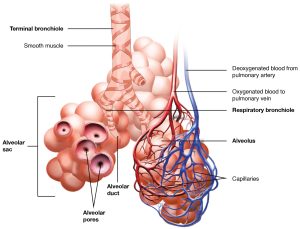
In contrast to the conducting zone, the respiratory zone includes structures that are directly involved in gas exchange. The respiratory zone begins where the terminal bronchioles join a respiratory bronchiole, the smallest type of bronchiole, which then leads to an alveolar duct, opening into a cluster of alveoli, as shown in Fig. 5.6.
Alveoli
An alveolar duct is a tube composed of smooth muscle and connective tissue that opens into a cluster of alveoli. An alveolus is one of the many small, grape-like sacs that are attached to the alveolar ducts.
An alveolar sac is a cluster of many individual alveoli that are responsible for gas exchange. An alveolus is approximately 200 μm (micrometres) in diameter, with elastic walls that allow the alveolus to stretch during air intake, which greatly increases the surface area available for gas exchange. Alveoli are connected to their neighbours by alveolar pores, which help maintain equal air pressure throughout the alveoli and lung (Fig. 5.7).

The alveolar wall consists of three major cell types: type I alveolar cells, type II alveolar cells, and alveolar macrophages. Taken together, the alveoli and capillary membranes form a respiratory membrane that is approximately 0.5 μm thick. Gases cross the respiratory membrane by simple diffusion, allowing oxygen to be picked up by the blood for transport and CO2 to be released into the air of the alveoli.
The following video provides a summary of the respiratory system anatomy and physiology.
(Osmosis.org, 2017)
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Anatomy and physiology. OpenStax. https://openstax.org/details/books/anatomy-and-physiology, licensed under CC BY 4.0
Reference
Osmosis from Elsevier. (2017, June 14). Anatomy and physiology of the respiratory system [Video]. YouTube. https://www.youtube.com/watch?v=0fVoz4V75_E
Image Credits (images are listed in order of appearance)
Respiratory system complete en.svg by LadyofHats, Public domain
Illu pharynx by Arcadian, Public domain
Anatomytool larynx and vocal cords English by Cenveo, CC BY 4.0
Trachea svg hariadhi by Hariadhi, CC BY-SA 4.0
202008 lung detailed by DataBase Center for Life Science (DBCLS), CC BY 4.0
2309 The Respiratory Zone by OpenStax College, CC BY 3.0
2310 Structures of the Respiratory Zone-a by OpenStax College, CC BY 4.0
a type of white blood cell involved in immune function