8.4 Endocrine System Medications
This section will discuss some of the more common medications that are used to treat hypothyroidism, hyperthyroidism, and diabetes mellitus, as well as common uses for corticosteroids. The mechanism of action of many of these medications is complicated, so we will only provide a basic overview of the medications in the categories below. Similarly to other chapters, a summary of all the medications discussed will be provided in a table at the end of the page.
Thyroid Replacement Medications
Levothyroxine (Synthroid) is a thyroid replacement medication used to treat hypothyroidism. Oral levothyroxine, shown in Fig. 8.9, is a synthetic T4 hormone that exerts the same physiological effect as endogenous T4, which means this medication can maintain normal T4 levels when a deficiency is present. Another medication available is liothyronine (Cytomel, Triostat), which also contains T4 and is a common medication for treating hypothyroidism (WebMD, 2023).

Thyroid replacement medications do not cure hypothyroidism, but rather supplement the lack, or low level of, T4, which means that treatment is lifelong. It is important to also monitor serum TSH levels before and during treatment to determine the effectiveness of the drug. Note that drug interactions may occur with several other medications, including anticoagulants and diabetic medications.
Anti-Thyroid Medications
Hyperthyroidism is often treated by thyroid surgery or with radioactive iodine (RAI) therapy. Patients are often given a radioactive oral medication, such as sodium iodide 131 (Iodotope), which collects in the thyroid cells and destroys the thyroid gland. This has little effect on the rest of body, but also destroys cancer cells if they are present in the thyroid. The patient must follow radiation precautions for a three-day period after RAI treatment to limit radiation exposure to others. This often includes staying in the hospital or away from others in the home. The end result of thyroid surgery or RAI treatment is often hypothyroidism, which is treated with thyroid hormone replacement therapy.
Propylthiouracil (PTU) is an anti-thyroid medication used to treat hyperthyroidism or to mimic the symptoms of hyperthyroidism in preparation for a thyroidectomy or radioactive iodine therapy. Propylthiouracil works by inhibiting the synthesis of thyroid hormones. This medication is administered orally, and the total daily dosage is usually given in three equal doses at approximately eight-hour intervals. Propylthiouracil can cause hypothyroidism, which makes it necessary to routinely monitor serum TSH levels and adjust the dose as needed to maintain optimal levels.
Adrenal Medications: Corticosteroids
Corticosteroids are common medications that are used to treat many different pathologies that have already been discussed in other chapters in this book. They are often used as a replacement therapy for adrenal insufficiency, as well as for the management of various dermatologic, rheumatologic, hematologic, and gastrointestinal (GI) disorders. Systemic corticosteroids are also often given for respiratory conditions and acute exacerbations of chronic obstructive pulmonary disease (COPD) and severe asthma.
There are various forms of corticosteriods and routes that corticosteroids can be given. Oral prednisone is the most widely used of the systemic corticosteroids and is generally used as an anti-inflammatory and immunosuppressive agent. Topical creams, such as hydrocortisone, are commonly used for itching, and its oral formulation is used to treat Addison’s disease. There are also various forms of injectable corticosteroids, such as methylprednisolone, which is used to treat inflammation associated with pathologies such as arthritis.
Some other examples of pathologies for which corticosteroids are administered:
- Adrenocortical insufficiency
- Rheumatoid arthritis
- Lupus erythematosus
- Psoriasis
- Contact dermatitis or drug hypersensitivity reactions
- Optic neuritis
- Asthma/COPD
- Ulcerative colitis
- Multiple sclerosis
Despite their beneficial effects, long-term systemic use of corticosteroids is associated with well-known adverse events, including osteoporosis and fractures, adrenal suppression, hyperglycemia and diabetes, cardiovascular disease and dyslipidemia, dermatological and GI events, psychiatric disturbances, and immunosuppression. Therefore, the lowest possible dose of corticosteroid should be used to control the condition requiring treatment to avoid the development of these adverse effects.

When a patient is taken off an oral dose of corticosteroids it is necessary to slowly reduce the dose. This is referred to as a tapered dosage, whereby the dose is slowly decreased over a number of days. Tapering the dosage is necessary to allow the adrenal cortex, which is suppressed by the large medication dose, to gradually begin to secrete its own cortisol again. Fig. 8.10 shows a common corticosteroid medication being given in a tapered dose, where the dosage and number of tablets decreases every day.
Key Concept
A few common suffixes seen with corticosteroids are -sone, -lone, -solone.
Examples: betamethasone, dexamethasone, hydrocortisone, prednisone
Diabetic Medication Classes: Insulins
Because patients with type 1 diabetes have absent, or near-absent, beta cell function in the pancreas, insulin treatment is essential. A number of different types of insulin and methods for administration are available. New technology is always evolving as it relates to the monitoring of blood sugars and administering insulin to patients to with type 1 diabetes. It is important to note that lifestyle modifications that improve health should also be emphasized, along with prescribing and administering insulin. Lifestyle modifications include healthy food choices to stabilize blood glucose levels, as well as daily exercise.

Insulin is most often given via the subcutaneous route, but in some cases in the hospital, it may be given intravenously if the patient’s condition requires it. Insulin, when administered subcutaneously, is given using a specialized insulin syringe that measures insulin in units (Fig. 8.11). This helps decrease errors and provides a more specific measurement of the amount of insulin being given to the patient. These insulin syringes are used to draw up insulin from vials of insulin, which are stored at the nursing station, elsewhere in the hospital, or in the patient’s home if the insulin is being self-administered.
Another option is an insulin pen, shown in Fig. 8.12, which is often used in the hospital setting, as well as for self-administration, to facilitate safe and accurate self-administration of insulin. The advantage of an insulin pen is that the insulin is pre-measured and stored in the pen and does not have to be drawn up from a vial.

There are also continuous computerized glucose monitors and pumps that provide automatic delivery of insulin to the patient. A number of these are available on the market, and Figs. 8.13 and 8.14 show some possible options. These devices decrease the need to regularly take blood glucose samples, and they administer insulin throughout the day and night.


Insulin is a high-alert medication that can be associated with significant patient harm when used incorrectly. In most healthcare settings, it is necessary for extra safety precautions to be taken, such as a double-check by two nurses before administering insulin to any patient. Patients on insulin therapy are at risk for hypoglycemia. It is essential for the healthcare provider, or the patient themself if at home, to monitor for signs of hypoglycemia and to intervene appropriately.
Types of Insulin
There are several different types of insulin that vary in terms of onset, peak, and duration.
Rapid-Acting Insulin
Rapid-acting insulins are administered with meals to mimic the effects of endogenous insulin release when food is eaten. Dosages of rapid-acting insulin vary greatly depending on individual patient factors as well as carbohydrate intake, premeal glucose levels, and anticipated activity during the day.
Rapid-acting insulins include insulin lispro (Humalog) and insulin aspart (Novolog) and are also available via inhalation (Afrezza). Because insulin lispro and insulin aspart act so quickly, as well as the potential for hypoglycemia, these insulins should be administered within 15 minutes before or right after eating a meal. Peak serum levels are seen 30 to 90 minutes after dosing. Inhaled insulin enters the bloodstream even faster, and effects are seen within one minute and peak in 30 to 60 minutes. Inhaled insulin is contraindicated in many patients, especially those with chronic lung disease such as asthma or COPD.
Short-Acting Insulins
Short-acting insulins are also given with meals to mimic the effects of endogenous insulin release when food is eaten. Dosages are individualized based on carbohydrate intake, premeal glucose levels, and activity levels. Short-acting inulin is often also referred to as regular insulin, and this is reflected in the abbreviation R found in many drug names, such as Humulin R and Novolin R.
Regular insulin, similar to other insulins, is generally administered subcutaneously, but it is the only insulin that can be administered intravenously as well. It is available in vials, as shown in Fig. 8.15, and insulin pens. Subcutaneous doses should be administered approximately 30 minutes before meals because this is when the onset of therapeutic action generally occurs. Peak effects occur in three hours, and the duration of effect is eight hours.

Intermediate-Acting Insulin
Intermediate-acting insulins are administered once or twice daily to mimic endogenous insulin levels. NPH insulin, also known as isophane insulin, is an example of an intermediate-acting insulin. Brand names include Humulin N or Novolin N. Mixtures of intermediate- and short-acting insulins are available in such mixes as Humulin 70/30 or Novolin 70/30. Not all insulins can come mixed, but it is possible with these forms of insulin. The onset, duration, and details of all the insulins discussed here, including some of the options for mixed insulins, are listed in Table 8.3 below.
Long-Acting Insulin
For those with type 1 diabetes, long-acting insulin should be combined with rapid- or short-acting insulin at mealtimes. Insulin glargine (Lantus) and insulin devemir (Levemir) are long-acting insulins given once or twice daily. Long-acting insulin has a relatively constant therapeutic effect over 24 hours, with no pronounced peak in comparison to NPH insulin. This can be seen in Fig. 8.16, which provides an illustration of the different types of insulin, their onset of action, and duration of effects within the body. Long-acting insulin should only be administered subcutaneously and is available in vials and insulin pens.
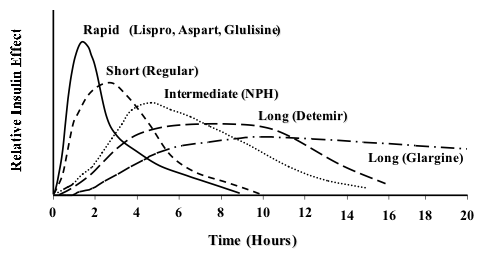
Table 8.3. Types of Insulin
| Class | Generic/Trade | Onset/Peak Effect/Duration |
| Rapid-Acting Insulin | insulin lispro (Humalog)
insulin aspart (Novolog) inhaled insulin (Afreeza)
|
Onset: 15–30 minutes
Peak effect: 1–3 hours Duration: 3–5 hours |
| Short-Acting Insulin | Humulin R
Novolin R |
Onset: 30 minutes
Peak effect: 3 hours Duration: 8 hours |
| Intermediate-Acting Insulin | Humulin N
Novolin N |
Onset: 1-2 hours
Peak effect: 6 hours Duration: up to 24 hours |
| Combination: Intermediate-Acting/Rapid-Acting | Humalog Mix 50/50
Humalog Mix 75/25 Novolog Mix 70/30 *First number is % of intermediate-acting insulin, second number is % of rapid-acting |
Onset: 15-30 minutes
Peak effect (50/50): 1–5 hours Duration: 11–22 hours
|
| Combination: Intermediate-Acting/Short-Acting | Humulin 70/30
Novolin 70/30 |
Onset: 30–90 minutes
Peak effect: 1.5–6.5 hours Duration: 18–24 hours |
| Long-Acting Insulin | insulin glargine (Lantus)
insulin detemir (Levemir) |
Onset: 3–4 hours
Peak effect: none Duration: >24 hours |
(Ernstmeyer & Christman, 2020)
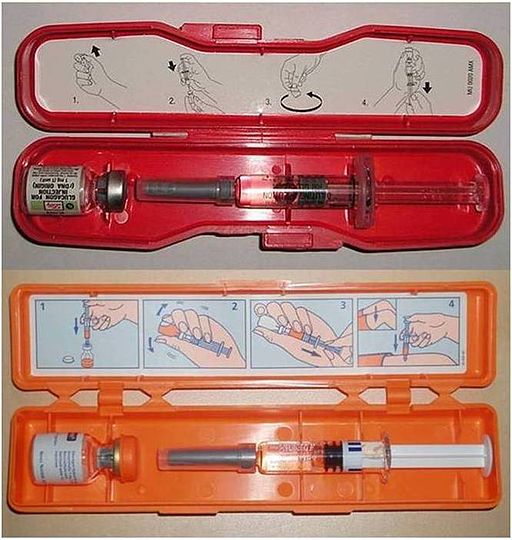
Glucagon
Glucagon (Glucagen) is indicated as a treatment for severe hypoglycemia, which may occur in patients with diabetes mellitus. Glucagon injections are used for patients who are unable to safely swallow carbohydrates to treat hypoglycemia because of the effects of severe hypoglycemia or possibly other medical conditions. Glucagon increases blood glucose concentration during an episode of hypoglycemia. It may be administered subcutaneously, intramuscularly, or intravenously. Peak therapeutic effects and glucose levels are seen within 13 to 20 minutes of subcutaneous or intramuscular injection. Fig. 8.17 shows an example of an emergency glucagon kit that can be used if a patient becomes hypoglycemic and cannot swallow carbohydrates to increase blood sugar.
Oral Antihyperglycemics
There are several different classes of oral antihyperglycemic drugs that are used in conjunction with a healthy diet and exercise for the management of type 2 diabetes.
Glipizide
Glipizide (Glucotrol) is an antihyperglycemic medication that works by stimulating insulin secretion from the beta cells of pancreatic islet tissue and is therefore dependent on functioning beta cells in the pancreatic islets. Peak plasma concentrations occur 1 to 3 hours after a single oral dose. It is important that patients understand that the medication, and other oral antidiabetic medications, help control episodes of hyperglycemia but do not cure diabetes.
Metformin
Metformin (Glucophage), shown in Fig. 8.18, is a antihyperglycemic that works by decreasing hepatic glucose production, decreasing the intestinal absorption of glucose, and improving insulin sensitivity by increasing peripheral glucose uptake and utilization. Metformin should be given in divided doses with meals with the therapeutic goal of decreasing both fasting plasma glucose and glycosylated hemoglobin levels to near normal by using the lowest effective dose.

Sitagliptin
Sitagliptin (Januvia) is an oral antihyperglycemic medication that works to increase insulin release and decrease glucagon levels in the blood. it is taken once daily, at the same time each day, and can be taken with or without food.
Glyburide
Glyburide (Diabeta) is an oral antihyperglycemic that used along with diet and exercise in Type 2 diabetes (WebMD, 2023). It belongs to the category of medications know as sulfonylureas. The drugs mechanism of action is to increase the bodies production of insulin and therefore lowers the blood sugar. Glyburide comes in various doses and it is important to only take what is prescribed. The best time to take glyburide is with your first morning meal daily (WebMD, 2023).
Table 8.4. Common Endocrine Medications
| Generic Name | Trade Name(s) | Reason for Administering |
| levothyroxine | Synthroid | Hypothyroidism |
| liothyronine | Cytomel, Triostat | Hypothyroidism |
| methimazole | Tapazole | Hyperthyroidism, Graves’ disease |
| propylthiouracil | Propacil | Hyperthyroidism |
| sodium iodide 131 | Iodotope | Hyperthyroidism, thyroid cancer |
| betamethasone | Celestone | Rheumatic disorders |
| dexamethasone | Decadron | Rheumatic problems, asthma, COPD |
| fludrocortisone | Florinef | Adrenal insufficiency |
| hydrocortisone | Cortef, Solu-Cortef | Adrenocortical insufficiency, rheumatoid arthritis, COPD, asthma |
| methylprednisolone | Medrol, Solu-Medrol | Inflammatory conditions, arthritis, lupus, ulcerative colitis |
| prednisolone | Pediapred, Prelone | Inflammatory conditions, autoimmune disorders |
| prednisone | Deltasone, Meticorten | Suppresses the immune system, decreases inflammation |
| triamcinolone | Aristocort, Kenalog | Skin diseases, allergies, rheumatic disorders |
| glucagon | Glucagen | Hypoglycemia |
| glipizide | Glucotrol | Type 2 diabetes |
| metformin | Glucophage | Type 2 diabetes |
| sitagliptin | Januvia | Type 2 diabetes |
| glyburide | Diabeta | Type 2 diabetes |
*Insulin is not included in this table.
(WebMD, 2023)
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/, licensed under CC BY 4.0
References
WebMD. (2023). Drugs & medications A–Z. https://www.webmd.com/drugs/2/index
Image Credits (images are listed in order of appearance)
Levothyroxine 25mcg Tablets by Ash, Public domain
Sandoz.Methylprednisolone.4mg by Anonymous, Public domain
Insulin syringe foto by Rehab Center Parus, CC BY-SA 4.0
Human insulin 100 IU-1ml pen yellow background by Wesalius, CC BY 4.0
Diabetic Type 1 adult man with insulin pump and CGM sensor by Medtd1, CC BY-SA 4.0
Insulin pump with infusion set by Mbbradford, Public domain
Human insulin 100IU-ml vial yellow background by Wesalius, CC BY 4.0
Insulin short-intermediate-long acting by Anne Peters, CC BY 3.0
Glucagon emergency rescue kits image by Mizi m, CC0 1.0 Universal
Metformin 500mg Tablets by Ash, Public domain
a condition in which the thyroid gland doesn't produce enough of certain hormones (T3 and T4)
originating from within an organism
a substance that opposes or prevents coagulation
a condition in which the thyroid gland produces too much of certain hormones (T3 and T4)
removal of the thyroid
a disorder that occurs when the adrenal glands do not produce enough of certain hormones, such as cortisol
under all the layers of the skin
pertaining to within the vein
low blood sugar
injected into the muscle