7.4 Hematological Medications
Hematological medications are used to treat various forms of the blood disorders that were discussed on the previous page (Mount Sinai, 2022). The medications listed below are some of the more common ones prescribed both in the hospital and in the community for patients with a history of clotting issues or who may be at risk for developing a blood clot. These medications are also often given to patients following an injury or treatment such as surgery, which might increase the patient’s chance of a blood clot. Long periods of immobility can also increase the chance of a blood clot developing, so patients may be given some of these medications if they will be spending a long period of time on bedrest, for example.
Heparin Sodium
Heparin sodium was the first anticoagulant developed and can be given either subcutaneously or intravenously. Heparin inhibits the activated coagulation factor X, which is involved in the clotting cascade. Heparin does not have fibrinolytic activity, so it will not break down existing clots. Only 20% to 30% of the dose exerts a therapeutic effect, which means that the dose must be higher than for other anticoagulants. Heparin is always measured in units and will only be seen measured as such in doctors’ orders and prescriptions. Fig. 7.8 below shows a vial of heparin and a syringe that would be used to draw up the medication. Often, heparin comes in a prefilled syringe because this decreases the chance of medication errors.
Intravenous heparin is commonly used to treat deep vein thrombosis (DVT) or a pulmonary embolism (PE). It is also indicated for use during an acute myocardial infarction. Subcutaneous heparin can be administered to prevent DVT or PE caused by atrial fibrillation and post-operatively to reduce the risk of the patient developing a blood clot. Because heparin is a high-alert medication, hospitals use several processes for storing and labelling the medication to help prevent errors. These processes can include an independent double-check of all orders and medications before they are given to the patient and having labels on the medication that indicate it is a high-alert medication.
Low-Molecular-Weight Heparin (LMWH)
As indicated by the name, low-molecular-weight heparin (LMWH) is related to heparin in that it is created by breaking apart the heparin molecule. Unlike heparin, where only 20% to 30% of the dose has a therapeutic effect, almost the whole dose of LMWH exerts that therapeutic effect. As a result, a lower dose is needed to see the same therapeutic effect as a larger dose of heparin. LMWH also works by inhibiting clotting factor X in the blood. It is always given subcutaneously and is measured in either units or milligrams. For example, dalteparin (Fragmin) and tinzaparin (Innohep) are measured in units, and enoxaparin (Lovenox) is measured in milligrams. If a patient is given an overdose of LMWH, protamine sulphate will reverse the effects.
An LMWH is often given for the prevention and treatment of deep vein thrombosis (DVT) and pulmonary embolism (PE). It can also be given to patients post-operatively or to those are hospitalized and at risk for developing a blood clot. In most cases, LMWH comes in a prefilled syringe, as can be seen in Fig. 7.9.

Key Concept
A common suffix seen in low-molecular-weight heparin medications is -parin.
Examples: dalteparin (Fragmin) and enoxaparin (Lovenox)
Both heparin and LMWH are often given in the hospital, and if the patient is required to continue on an anticoagulant after they are discharged, they are often switched to an oral form of anticoagulant such as warfarin.
Warfarin
Warfarin (Coumadin) is an oral anticoagulant and is measured in milligrams (mg). It is available in various strengths, and each of these strengths comes in a different colour to help prevent errors when patients self-administer different dosages at home (Fig. 7.10). Close monitoring of prothrombin time (PT) or international normalized ratio (INR) is required when patients are taking warfarin. It acts by inhibiting the synthesis of vitamin-K-dependent clotting factors, which include factors II, VII, IX, and X, and other anticoagulant proteins.
Patients may take warfarin to prevent and treat venous thrombosis, such as DVT, and pulmonary embolus (PE). Patients with atrial fibrillation may take the medication to prevent blood clots from forming and to reduce the risk of death associated with recurrent myocardial infarctions.

Key Concept
Certain foods and vitamins can either increase or decrease the effects of warfarin. For example, vitamin K can produce an effect referred to as antagonism, whereby ingesting vitamin K can decrease the effects of the medication. As a result, a patient’s risk of blood clots could increase because the effects of warfarin are decreased.
On the other hand, cranberries, garlic, and grapefruit can increase the effects of warfarin. This is known as synergism because these foods increase the effects of this particular medication. This could result in an increased risk of hemorrhage because the patient’s blood would not clot when it should.
Platelet Aggregation Inhibitor (Antiplatelet) Drugs
Medications in this category prevent platelets from clumping together (aggregating), adhering to the site of an injury, and beginning to form a clot. They are given to patients with peripheral arterial disease or a history of recent myocardial infarction (MI) or cerebrovascular accident (CVA), and to those at risk of having an MI or CVA. They are also given if a patient is having heart surgery such as a valve or stent replacement or an angioplasty.
Acetylsalicylic acid (aspirin) and clopidogrel (Plavix) are common examples of antiplatelet medications. Low-dose aspirin (81 mg) is taken daily by many patients for its antiplatelet effect. However, aspirin can also be taken for other reasons because of its anti-inflammatory, analgesic, and anti-pyretic effects.
Selective Xa Inhibitor and Thrombin Inhibitor Medications
Selective inhibitors of factor Xa indirectly inhibit platelet aggregation induced by thrombin. Selective Xa inhibitors are used to prevent blood clots in patients with unstable angina and those having angioplasty or a joint replacement. These medications are also given to patients to prevent or treat deep vein thrombosis and pulmonary embolism. Thrombin inhibitor medications are similar to selective Xa inhibitors and are indicated for the same patient population, but they inhibit thrombin instead of factor Xa. Rivaroxaban is an example of a selective Xa inhibitor, and dabigatran is a thrombin inhibitor.
Thrombolytic Medications
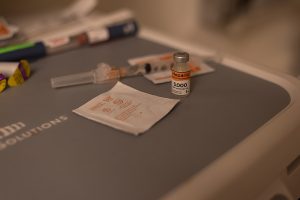
Anticoagulants will not dissolve or break apart a clot that has already developed. Thrombolytic medication is required in the acute treatment of a myocardial infarction (MI), cerebrovascular accident (CVA), or pulmonary embolism (PE). Thrombolytics will break apart clots rapidly once administered. Alteplase (tPA) is a common thrombolytic that is used for the above-mentioned pathologies. Fig. 7.11 is an image of a patient’s hand before and after treatment with a thrombolytic for a blood clot in the hand. You can see circulation returning to the patient’s hand in the second part of the image.
Anemia
As previously mentioned, there are a number of causes for anemia, and treatment will depend on the causative factor. For example, iron-deficiency anemia can be treated with supplemental iron. Fig. 7.12 shows an example of an oral form of supplemental iron medication that can be given for this type of anemia. Medications with “Fe” or “ferrous” in the name are often used to treat iron-deficiency anemia and examples are listed in Table 7.1.

Table 7.1. Common Medications for Iron-Deficiency Anemia
| Generic Name | Trade Name |
| ferrous fumarate | Ferro-Sequels |
| ferrous sulfate | Feosol, Fer-In-Sol, Slow FE |
| ferrous gluconate | Fergon |
(WebMD, 2022)
Because vitamin B12–deficiency anemia and folate-deficiency anemia often occur together, they are usually treated in a similar manner (John Hopkins Medicine, 2022). Vitamin B12–deficiency anemia is a condition in which the body lacks enough vitamin B12, which is necessary for the development of healthy red blood cells. Folic acid, also called folate, is another B vitamin that is needed for red blood cell development (John Hopkins Medicine, 2022). These vitamin deficiencies cause red blood cells to be oval and very large rather than developing normally. This results in the bone marrow making fewer red blood cells, and the red blood cells often die sooner than normal. Treatment typically includes vitamin B12 injections and oral folic acid supplements (John Hopkins Medicine, 2022).
Table 7.2. Common Hematologic Medications
| Generic Name | Trade Names |
| heparin sodium, heparin | Heparin |
| dalteparin | Fragmin |
| tinzaparin | Innohep |
| enoxaparin | Lovenox |
| warfarin | Coumadin, Jantoven |
| acetylsalicylic acid (ASA) | aspirin, Bayer, Ecotrin |
| clopidogrel | Plavix |
| rivaroxaban | Xarelto |
| dabigatran | Pradaxa |
| alteplase (tPA) | Alteplase |
(WebMD, 2022)
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/ licensed under CC BY 4.0
References
John Hopkins Medicine. (2022). Vitamin B12 deficiency anemia. https://www.hopkinsmedicine.org/health/conditions-and-diseases/vitamin-b12-deficiency-anemia
Mount Sinai. (2022). Hematologic disorders. https://www.mountsinai.org/care/surgery/services/pediatric-surgery/conditions-we-treat/hematologic-disorders
WebMD. (2022). Drugs and medications A–Z. https://www.webmd.com/drugs/2/index
Image Credits (images are listed in order of appearance)
Heparin_1 by Sixflashphoto, CC BY-SA 4.0
Thrombosespritze_04_(fcm) by Frank C. Müller, CC BY-SA 4.0
Warfarintablets5-3-1 by Gonegonegone, CC BY-SA 3.0
Angiograph_before_and_after_thrombolytic_therapy_in_a_case_of_thrombosis_on_the_hand by Ipaktchi K, CC BY 2.0
Retafer+ by Styroks, CC BY-SA 4.0
under all the layers of the skin
pertaining to within the vein
a test that evaluates blood clotting
a test that measures the time required for blood to clot; abbreviated as INR
a decrease in the therapeutic effects of a medication
an increase in the therapeutic effects of a medication
medications used to dissolve a major clot quickly