9.4 Nervous System Medications
The most common medications and medication categories for conditions of the nervous system are discussed below. Some conditions, such as multiple sclerosis, are very complex to treat and involve many medications, and as such, those pathologies and the medications used to treat them are not included below.
Anticonvulsants
Medications used for seizures are called anticonvulsants. Anticonvulsant medications stabilize cell membranes and suppress the abnormal electric impulses in the cerebral cortex. These medications prevent seizures but do not provide a cure. Anticonvulsants are classified as central nervous system depressants. There are many types of medications used to treat seizures, including phenytoin (Dilantin), phenobarbital (Luminal), benzodiazepines, carbamazepine (Tegretol), valproate (valproic acid), and levetiracetam (Keppra).
There are three main pharmacological effects of anticonvulsant medications. First, they increase the threshold of activity in the motor cortex, making it more difficult for nerves to become excited. Second, they limit the spread of a seizure discharge from its origin by suppressing the transmission of impulses from one neuron to the next. Third, they decrease the speed of nerve impulse conduction within a given neuron.
Hydantoin Medications
Phenytoin (Dilantin), which was discovered in 1938, is categorized as a hydantoin medication. It was the first anti-seizure medication and is still being used to control seizures. Phenytoin lessens the incidence of seizures by interfering with sodium channels in the brain, resulting in a reduction of sustained high-frequency neuronal discharges.
Phenytoin has a narrow therapeutic drug level, usually 10–20 mcg/mL, so serum drug monitoring is required. Serum levels of phenytoin sustained above the therapeutic range may produce delirium, psychosis, and encephalopathy, which means it is important, at the first sign of acute toxicity, for serum levels to be immediately checked.
Key Concept
A common suffix for hydantoin medications for epilepsy is -toin.
Examples: ethotoin (Peganone), fosphenytoin (Cerebyx), phenytoin (Dilantin)
Benzodiazepine Medications
Key Concept


Barbiturate Medications
Key Concept
Levetiracetam
Levetiracetam is indicated as adjunctive therapy in the treatment of partial onset seizures in patients with epilepsy and is generally well tolerated. The exact mechanism of action is unknown, but this medication may interfere with sodium, calcium, potassium, or GABA transmission. Withdrawal seizures may occur if levetiracetam is stopped abruptly.
Gabapentin
Gabapentin is indicated as an adjunctive treatment for partial seizures, but it is most commonly used to treat neuropathic pain. An example of neuropathic pain is tingling or burning in the lower extremities that often occurs in patients with diabetes. The exact mechanism of action is unknown.
Antiparkinson Medications
Parkinson’s disease is believed to be related to an imbalance of dopamine and acetylcholine and a deficiency of dopamine in certain areas of the brain, so drug therapies are aimed at increasing levels of dopamine and/or antagonizing the effects of acetylcholine. Drug therapy does not cure the disease but is used to slow the progression of symptoms. Common medications used to treat Parkinson’s disease are carbidopa/levodopa, selegiline, and amantadine.
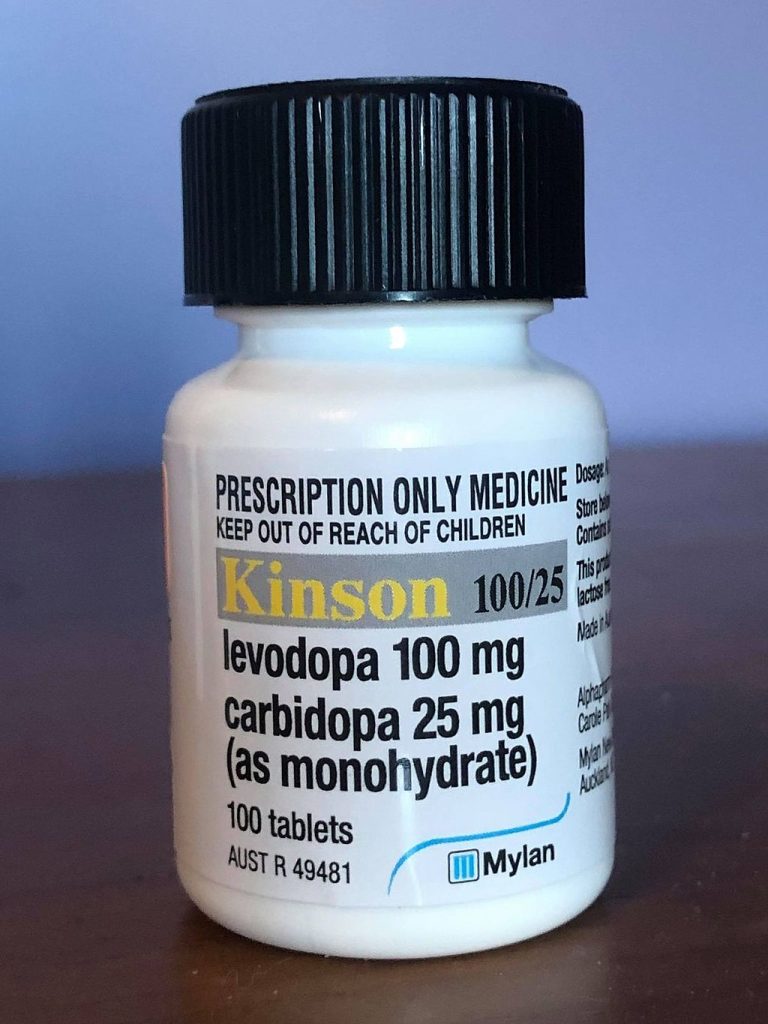
Carbidopa/Levodopa
Carbidopa/levodopa, shown in Fig. 9.12, is the most common drug used to treat Parkinson’s disease and is usually started as soon as the patient becomes functionally impaired. The administration of dopamine is ineffective in the treatment of Parkinson’s disease because it does not cross the blood-brain barrier, but levodopa, the metabolic precursor of dopamine, does cross the blood-brain barrier and presumably is converted to dopamine in the brain. Carbidopa is combined with levodopa to help stop the breakdown of levodopa. Additionally, the incidence of levodopa-induced nausea and vomiting is less when levadopa is combined with carbidopa.
Selegiline
Selegiline is often used in conjunction with carbidopa/levodopa when patients demonstrate a deteriorating response to that treatment; it is helpful for controlling symptom fluctuations. Selegiline inhibits MAO-B, blocking the breakdown of dopamine. There is no evidence from controlled studies that selegiline has any beneficial effect in the absence of concurrent levodopa therapy.
Amantadine
Amantadine is used in the early stages of Parkinson’s disease, but it can be effective in moderate or advanced stages in reducing tremors and muscle rigidity. The exact mechanism of action is unknown, but it is an antiviral drug that acts on dopamine receptors.
None of these medications can cure Parkinson’s, and over time, it is not uncommon for tolerance to these medications to increase, so the dose often needs to be increased to maintain the same therapeutic effect. Eventually, the side effects also become worse, so at a certain point, the physician may place the patient on a “drug holiday.” This means the patient stops taking medications for a few days, then restarts at a lower dose.
Alzheimer’s Medications
Insomnia Medications
Nonbarbiturate Hypnotic or Sedative Medications
- Chloral hydrate (Somnote)
- Zopiclone (Imovane)
- Zolpidem (Ambien, Intermezzo, Zopimist)
Anti-Anxiety (Benzodiazepines) and Antidepressant Medications
- Anti-anxiety medications:
- Flurazepam (Dalmane)
- Temazepam (Restoril)
- Triazolam (Halcion)
- Antidepressant drugs for insomnia:
- Doxepin (Silenor)
- Trazodone (Oleptra)
Melatonin

| Generic | Trade | Reason For Administering |
| carbamazepine | Tegretol | seizure disorders |
| valproate | Valproic acid | seizure disorders |
| ethotoin | Peganone | seizure disorders |
| fosphenytoin | Cerebyx | seizure disorders |
| gabapentin | Neurontin | seizure disorders |
| levetiracetam | Keppra | seizure disorders |
| mephobarbital | Mebaral | seizure disorders |
| phenobarbital | Luminal | seizure disorders |
| phenytoin | Dilantin | seizure disorders |
| amantadine | Gocovri | Parkinson’s disease |
| carbidopa/levodopa | Sinemet | Parkinson’s disease |
| selegiline | Eldepryl, Emsam | Parkinson’s disease |
| donepezil | Aricept | Alzheimer’s disease/dementia |
| razadyne | Galantamine | Alzheimer’s disease/dementia |
| rivastigmine | Exelon | Alzheimer’s disease/dementia |
| tacrine | Cognex | Alzheimer’s disease/dementia |
| chloral hydrate | Somnote | Insomnia |
| zopiclone | Imovane | Insomnia |
| zolpidem | Ambien, Intermezzo, Zopimist | Insomnia |
| flurazepam | Dalmane | Insomnia/anxiety |
| temazepam | Restoril | Insomnia/anxiety |
| triazolam | Halcion | Insomnia/anxiety |
| doxepin | Silenor | Insomnia/depression |
| trazodone | Oleptra | Insomnia/depression |
(WebMD, 2022)
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/ licensed under CC BY 4.0
References
Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Anatomy and physiology. OpenStax. https://openstax.org/details/books/anatomy-and-physiology licensed under CC BY 4.0
WebMD. (2022). Drugs & medications A–Z. https://www.webmd.com/drugs/2/index
Image Credits (images are listed in order of appearance)
Loratsepaamiin_perustuvia_lääkkeitä by Melissan, Public domain
Lorazepam2mgmLvial by Stickpen, Public domain
Medicationlevodopa by Revion101, CC BY-SA 4.0
Melatonin_prescription by Murrur, CC BY-SA 3.0
when another medication is given alongside or in addition to a primary medication used to treat a particular condition