8.3 Endocrine Pathologies
A number of pathologies can affect the endocrine system; however, the primary focus for this section will be the pathologies that result from issues with the three major endocrine glands that are the focus of this chapter: the adrenal glands, the pancreas, and the thyroid gland. A few other common endocrine pathologies that do not involve these three glands are also included in this section.
Common Pathologies
Acromegaly: This disorder affects adults and is caused by abnormally high levels of growth hormone that result in increased growth of the bones in the face, hands, and feet (Betts et al., 2013).
Addison’s disease: This condition is caused by the hyposecretion of corticosteroids, which also results in low blood glucose levels and low blood sodium levels. An Addisonian crisis is a life-threatening condition that presents with severely low blood pressure as a result of low corticosteroid levels (Betts et al., 2013). Addison’s disease is a type of adrenal insufficiency and is characterized by the adrenal glands releasing too little cortisol.
Cushing’s syndrome: This pathology results from excessive production of the hormone cortisol. The signs and symptoms are rapid weight gain, depression, anxiety, high blood sugar, a moon-shaped face, and fatigue. Individuals also experience weak muscles and bone pain (Betts et al., 2013).
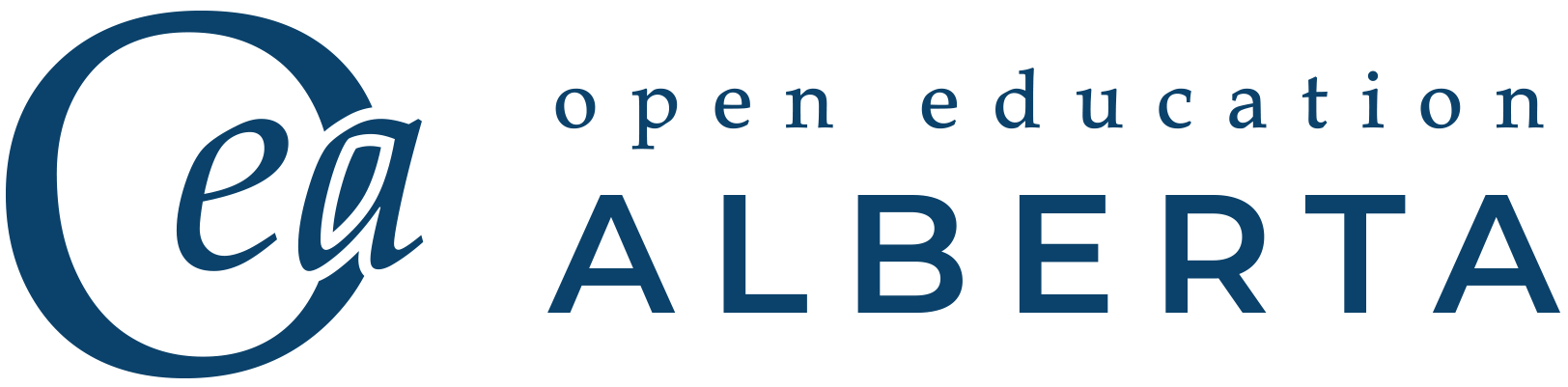
Diabetes mellitus: Dysfunction of insulin production and secretion, as well as the target cells’ responsiveness to insulin, can result in this condition. It is a common disease that affects the ability of the body to produce and use insulin. When diabetes mellitus goes untreated or is uncontrolled, blood glucose levels are consistently elevated. This can eventually lead to complications such as diabetic retinopathy, neuropathy, arteriosclerosis, increased risk of infections, ketoacidosis, and even death. Fig. 8.6 is an illustration of the beta cells and the pancreatic islets in the pancreas, both of which play an integral role in the regulation of blood glucose levels.
There are two main forms of diabetes mellitus:
- Type 1 diabetes is an autoimmune disease that affects the beta cells of the pancreas. The beta cells in people with type 1 diabetes do not produce insulin, so these individuals require synthetic insulin, which is administered by injection or infusion. The most common means of administering insulin is through a subcutaneous injection. This form of diabetes is often diagnosed in childhood and was previously known as insulin dependent diabetes mellitus (IDDM).
- Type 2 diabetes accounts for approximately 95% of all cases of diabetes. It is acquired later in life, and factors such as poor diet and inactivity greatly increase a person’s risk of developing this condition. In type 2 diabetes, the body’s cells become resistant to the effects of insulin. In response, the pancreas increases its insulin secretion, but over time, the beta cells become exhausted. In many cases, type 2 diabetes can be controlled by moderate weight loss, regular physical activity, and a healthy diet. However, if blood glucose levels cannot be controlled, oral diabetic medication is prescribed, and eventually those with type 2 diabetes may even require insulin. This type of diabetes used to be referred to as non-insulin dependent diabetes mellitus (NIDDM).
Table 8.2. Symptoms of Hypoglycemia and Hyperglycemia
| Hypoglycemia | Hyperglycemia |
| Shaky or jittery | Blurred vision |
| Sweaty | Increased thirst and frequent urination |
| Hungry | Feeling weak and tired |
| Headache | Fruity-smelling breath |
| Blurred vision | Dry mouth |
| Dizzy or lightheaded | Nausea and vomiting |
| Confused or disoriented | Abdominal pain |
| Fast or irregular heartbeat | Shortness of breath |
| Seizures or convulsions (jerky movements) | Confusion |
| Unconsciousness | Unconsciousness |
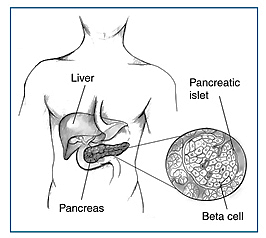
Hypothyroidism: This condition is marked by low levels of thyroid hormones, which can result from different causes. Treatment varies depending on the causative factors contributing to the patient’s condition. Hypothyroidism is characterized by a low metabolic rate, weight gain, cold extremities, constipation, reduced libido, menstrual irregularities, and reduced mental activity. This condition requires long-term thyroid hormone replacement therapy. Some of the potential causes include the following:
- Dietary iodine deficiency can result in the impaired ability to synthesize T3 and T4, which can then lead to a number of severe disorders. For much of the world’s population, foods do not provide adequate levels of iodine because the amount varies according to the level in the soil in which the food was grown, as well as irrigation and the fertilizers used. Therefore, the primary source of dietary iodine in many countries is iodized salt. When the body cannot produce T3 and T4, thyroid-stimulating hormone (TSH) is secreted in increasing amounts. As a result, the thyroid gland increases in size, resulting in a goiter, which is shown in Fig. 8.7. Iodine deficiency can also result in impaired growth and development, decreased fertility, and prenatal and infant death.
- In areas of the world with access to iodized salt, dietary deficiency of iodine is rare. Instead, inflammation of the thyroid gland or low blood levels of thyroid hormones is a common cause of hypothyroidism.
Hyperthyroidism: This condition is characterized by abnormally elevated blood levels of thyroid hormones and is often caused by a pituitary or thyroid tumour. It can also result from an autoimmune reaction referred to as Graves’ disease, in which antibodies overstimulate the follicle cells of the thyroid gland. Hyperthyroidism can lead to an increased metabolic rate, excessive body heat and sweating, diarrhea, weight loss, tremors, and increased heart rate. The person’s eyes may bulge, called an exophthalmic goiter (Fig. 8.8) because antibodies produce inflammation in the soft tissues of the eye orbits.

Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/, licensed under CC BY 4.0
References
Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Anatomy and physiology. OpenStax. https://openstax.org/details/books/anatomy-and-physiology, licensed under CC BY 4.0
Image Credits (images are listed in order of appearance)
Pancreas insulin beta cells by National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Health Information, Public domain
A woman suffering from Goiter by myUpchar, CC BY-SA 4.0
Proptosis and lid retraction from Graves’ Disease by Jonathan Trobe, CC BY 3.0
a disorder that occurs when the adrenal glands do not produce enough of certain hormones, such as cortisol
disease of the retina
disease of the nerves
hardening of the arteries
a serious complication from diabetes that results from the body breaking down fat as fuel, which causes a build-up of acids called ketones in the bloodstream and can be life threatening
under all the layers of the skin