12.2 Antimicrobial Basics
Before we learn about medications that are used to treat infections in patients, we must first understand the basics of microbiology. Let’s begin with a review of bacteria. Bacteria are found in nearly every habitat on earth, including within and on humans. Most bacteria are harmless or considered helpful, but some are pathogens. A pathogen is defined as an organism causing disease to its host. Pathogens, when overgrown, can cause significant health problems or even death for patients.
The term antimicrobial most often refers to medications used to treat bacteria, but it also includes medications used to treat viruses and fungi. We will discuss some important concepts concerning antimicrobials throughout this chapter. These include the fact that bacteria may be identified when a patient has an infection by using a culture and sensitivity test or a gram stain test. Antimicrobials may be classified as broad-spectrum or narrow-spectrum, based on the variety of bacteria they treat effectively. Additionally, antibiotics may be bacteriostatic or bactericidal in terms of how they target bacteria. Finally, the mechanism of action is also considered in the selection of an antibiotic to treat a particular infection.
Culture and Sensitivity
When a patient presents signs or symptoms of an infection, healthcare providers will begin the detective work needed to identify the source of the infection. A culture is a test performed to examine different body substances for the presence of bacteria or fungi (Parker et al., 2016). These culture samples are commonly collected from a patient’s blood, urine, sputum, feces, or wound bed. Nurses are typically responsible for the collection of culture samples and must be conscientious about collecting the sample prior to the administration of antibiotics. Antibiotic administration prior to a culture being taken can result in delayed identification of the organism and complicate the patient’s recovery. Once culture samples are collected, they are then incubated in a solution that promotes bacterial or fungal growth and spread onto a special culture plate (Fig. 12.1) (Parker et al., 2016). Specialists then monitor the culture for signs of organism growth to aid in the diagnosis of the infectious pathogen. A sensitivity analysis is often performed to select an effective antibiotic to treat the microorganism. If the organism shows resistance to the antibiotic used in the test, that antibiotic will not provide effective treatment for the patient’s infection.

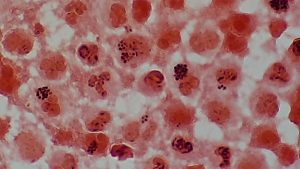
Gram Positive vs. Gram Negative
A gram stain is another type of test used to help classify pathogens (Fig. 12.2). Gram stains are useful for quickly identifying whether bacteria are gram positive or gram negative, based on the staining patterns of their cellular walls. Identification of bacteria as gram positive or gram negative helps the healthcare provider quickly select an appropriate antibiotic to treat an infection.
Broad-Spectrum vs. Narrow-Spectrum Antimicrobials
Spectrum of activity is one of the factors that healthcare providers use when selecting antibiotics to treat a patient’s infection. A narrow-spectrum antibiotic targets only specific types of bacterial pathogens (Parker et al., 2016). For example, some narrow-spectrum medications only target gram-positive bacteria, but others target only gram-negative bacteria. If the pathogen causing the infection has been identified in a culture and sensitivity test, it is best to use a narrow-spectrum antimicrobial and minimize collateral damage to the normal microbacteria.
A broad-spectrum antibiotic targets a wide variety of bacterial pathogens, including both gram-positive and gram-negative species, and is frequently used to cover a wide range of potential pathogens while waiting for laboratory identification of the infecting pathogen. Broad-spectrum antibiotics are also used for polymicrobial infections (a mixed infection with multiple bacterial species) or as prophylactic prevention of infections with surgery or invasive procedures. Finally, broad-spectrum antibiotics may be selected to treat an infection when a narrow-spectrum drug fails because of the development of medication resistance by the target pathogen (Parker et al., 2016).
One risk associated with using broad-spectrum antibiotics is that they also target a broad spectrum of normal microbacteria, which can cause diarrhea. They also increase the risk of a superinfection, a secondary infection in a patient who has a pre-existing infection. A superinfection develops when the antibacterial intended for the pre-existing infection kills the protective microbiota, allowing another pathogen that is resistant to the antibacterial to proliferate and cause a secondary infection. Common examples of superinfections that develop as a result of antibiotic use include yeast infections (candidiasis) and pseudomembranous colitis caused by Clostridium difficile (C. diff), which can be fatal (Parker et al., 2016).
Antibacterial Actions
When a provider selects an antibacterial medication, it is important to consider how and where the medication will target the bacteria. Antibacterial medications can be either bacteriostatic or bactericidal in their interactions with the offending bacteria. Bacteriostatic medications cause bacteria to stop reproducing; however, they may not ultimately kill the bacteria. In contrast, bactericidal medications kill their target bacteria.
The decision about whether to use a bacteriostatic or bactericidal drug often depends on the type of infection and the overall immune status of the patient. In a healthy patient with strong immune defences, both bacteriostatic and bactericidal medications can be effective in achieving a clinical cure. However, when a patient is immunocompromised, a bactericidal medication is essential for the successful treatment of infections. Regardless of the immune status of the patient, life-threatening infections such as acute endocarditis require the use of a bactericidal medication to eliminate all the offending bacteria (Parker et al., 2016).
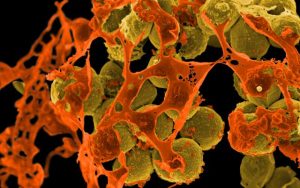
Medication Resistance
Although there are numerous medications available to treat infections, greater limitations in effectiveness are being seen. This is because some bacteria have developed resistant strains that are immune to certain antibiotic medications. This happens because antibiotic medications have been so widely prescribed, and they are often prescribed for conditions that do not warrant antibiotic medication use. For example, methicillin-resistant Staphylococcus aureus (MRSA) causes serious and sometimes fatal infections in hospitalized patients, and now has been found in patients who are in other types of healthcare facilities and even in homes and in the community. Other antibiotic-resistant organisms (AROs) include bacteria such as vancomycin-resistant Enterococcus (VRE), which is resistant to the antibiotic vancomycin (Fig. 12.3).
In many countries around the world, antibiotics are self-administered by patients at home. Unfortunately, many patients stop taking antibiotics once their symptoms go away and they feel better. If a 10-day course of treatment is prescribed, many patients only take the medication for five or six days, unaware of the negative consequences of not completing the full course of treatment.
The problem: A shorter course of treatment not only fails to kill the target organisms to the expected levels but also helps create drug-resistant variants within the body. A patient’s nonadherence amplifies drug resistance when the recommended course of treatment is long.
For example, treatment for tuberculosis (TB) has a recommended treatment regimen lasting from six months to a year. The Centers for Disease Control (CDC) estimates that about one-third of the world’s population is infected with TB, most living in underdeveloped or underserved regions where antimicrobial medications are available over the counter. In such countries, there may be even lower rates of adherence than in developed areas. Nonadherence leads to antibiotic resistance and more difficulty in controlling pathogens. As a direct result, the emergence of multidrug-resistant strains of TB is becoming a huge problem.
The overprescription of antimicrobials also contributes to antibiotic resistance. Patients often demand antibiotics for diseases that do not require them, such as viral colds and ear infections. Pharmaceutical companies aggressively market medications to physicians and clinics, making it easy for them to give free samples to patients, and some pharmacies even offer certain antibiotics free to low-income patients with a prescription.
In recent years, various initiatives have aimed to educate patients, parents, and clinicians about the use of antibiotics. However, previous studies have shown that the parental expectations for antimicrobial prescriptions for children has actually increased.
This is a complex issue with no clear, easy solution. However, what is clear is that extensive education regarding the judicious and complete use of medications to increase adherence and decrease the opportunity for antimicrobial resistance is required (Parker et al., 2016).
The video below provides an overview of antibiotic resistance and the increase in “superbugs.”
(Be Smart, 2015)
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/, licensed under CC BY 4.0
References
Be Smart. (2015, April 15). Antibiotic resistance and the rise of superbugs [Video]. YouTube. https://www.youtube.com/watch?v=fyRyZ1zKtyA
Parker, N., Schneegurt, M., Thi Tu, A.-H., Lister, P., & Forster, B. M. (2016). Microbiology. OpenStax. https://openstax.org/details/books/microbiology?Book%20details, licensed under CC BY 4.0
WebMD. (2023). Drugs & medications A–Z. https://www.webmd.com/drugs/2/index
Image Credits (images are listed in order of appearance
antibiotic sensitivity and resistance by Dr Graham Beards, CC BY-SA 4.0
Plenty of Gram positive cocci in singles, pair and clusters in Gram stained smear of wound drainage by Ajay Kumar Chaurasiya, CC BY-SA 4.0
Methicillin-resistant Staphylococcus aureus (MRSA) Bacteria by NIAID/NIH, Public domain
an organism that causes disease to its host
antibiotics that work for many types of bacterial infections
antibiotics that target only specific types of bacterial pathogens
antibiotics that fight off bacteria by slowing their growth
antibiotics that kill bacteria