1.4 Parenteral Medication Forms and Routes
The parenteral route sometimes refers to any route of administration other than oral, but more often, it refers to a route that involves injecting medication into the body. This section will discuss all parenteral routes of administration that involve injecting medication or fluids. There are benefits and drawbacks to all these routes, and many factors must be considered when determining the best route for a given medication.
Subcutaneous (sc) Route
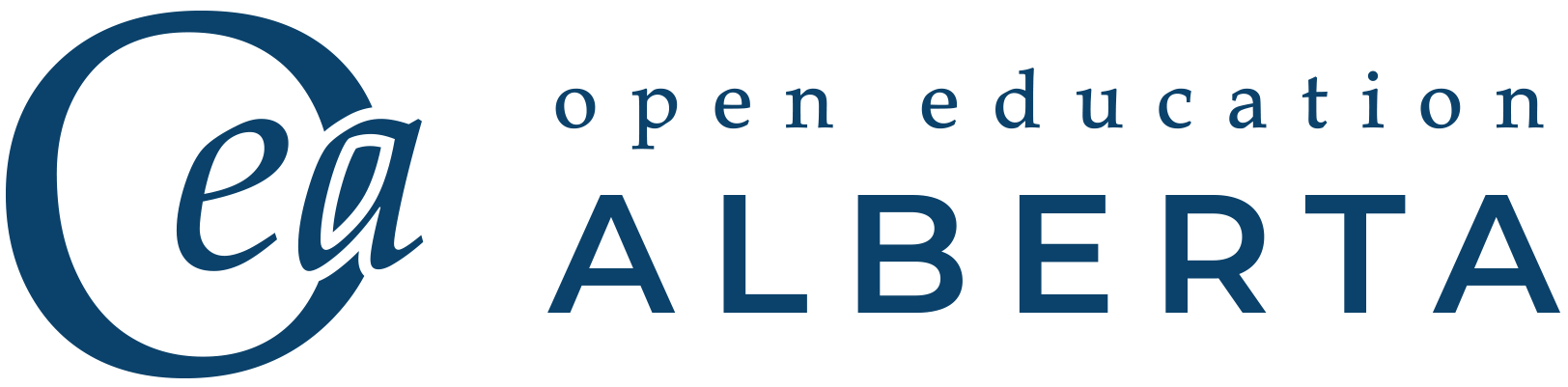
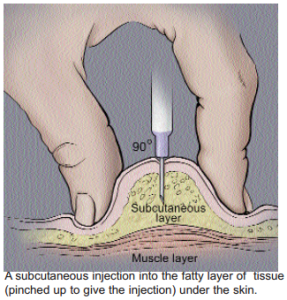
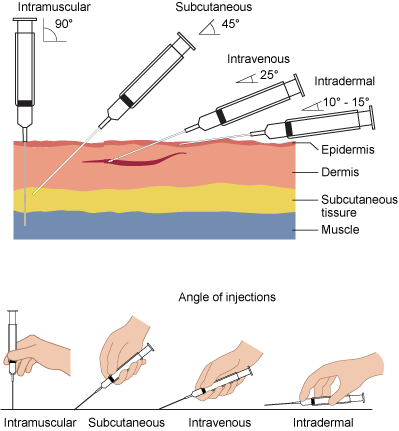
The subcutaneous route (abbreviation sc) delivers medication into the deepest layer of the skin, which is composed of fats and tissues (Ernstmeyer & Christman, 2020). The medication is injected with a syringe and needle and has a relatively predictable rate of absorption. The benefit of this route is that the therapeutic effects last longer than other routes, such as the intravenous route, for example. The location and means of injecting the medication make it easier for patients to self-administer at home compared to other routes, such as the intramuscular route. One of the drawbacks of the subcutaneous route compared to oral or other noninvasive routes is the possibility of infection because the patient’s skin is pierced. Also, the therapeutic effects generally take longer to take effect as compared to medications administered via the intravenous route, so the subcutaneous route is not ideal in an emergency (Ernstmeyer & Christman, 2020). Fig. 1. 21 provides an example of how subcutaneous injections are administered, and Fig. 1.22 shows locations where subcutaneous injections can be given.
Intramuscular (IM) Route
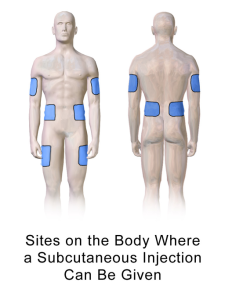
The intramuscular route (abbreviation IM) delivers medication into a patient’s muscle (Ernstmeyer & Christman, 2020). The therapeutic effects tend to last longer via this route as compared to the subcutaneous route. However, the main drawback for this route is that because of the location and the technique required to do the injection, it is highly unlikely that a patient would be able to self-administer medication at home. There is also a higher chance of infection because the needle is inserted more deeply and at a 90° angle into the tissue, as can be seen in Fig. 1.23. This route is ideal for administering many medications as well as vaccines (Ernstmeyer & Christman, 2020).
Medication Forms
Medication that is to be administered by either of the routes shown above and, in some cases, intravenously, usually comes in a vial or ampoule and is drawn up into a syringe (Ernstmeyer & Christman, 2020).
Vials are shown in Fig.1.24 and can be used multiple times because the medication is drawn up through a sealed stopper on the top. The medication may come as a liquid in the vial or a powder that is then reconstituted with sterile water or normal saline, then shaken to mix the contents.
Fig. 1.25 shows an ampoule that contains liquid medication; the ampoule is opened by breaking the top, and the medication withdrawn with a syringe (Ernstmeyer & Christman, 2020). Ampoules cannot be reused, so any unused medication must then be discarded as per the hospital’s policy.


Intradermal Route
The intradermal route is less common for administering medications and involves injecting a medication or other substance into the dermis, which is right below the epidermis. This route is often used for tuberculosis and allergy testing, but it is also used to inject local anesthetics (Ernstmeyer & Christman, 2020), for example, if a patient requires stitches. Fig. 1.26 demonstrates how an intradermal injection is completed, and Fig.1. 27 provides a comparison of four different parental routes.

Intravenous (IV) Route
The intravenous route (abbreviation IV) delivers medication through an intravenous line that is connected to a small catheter in a patient’s vein. The therapeutic effects of medication given intravenously occur faster as compared to intramuscular and subcutaneous injections but do not last as long. However, the immediate therapeutic effect makes it a desirable route in an emergency, where it is important for the patient to receive the medication as quickly as possible. There can also be complications with this route if the intravenous catheter dislodges from the vein. This is called extravasation, and in this situation, the fluid from the intravenous line flows into the subcutaneous tissue rather than the vein. This can become very uncomfortable for the patient, and the area around the intravenous site will begin to swell. Another complication is called vesicant, whereby the medication in the intravenous line irritates the skin, causing blisters or necrosis, when it contacts the subcutaneous tissue. When this is a concern for a particular medication, the intravenous site should be monitored regularly for any issues.
The equipment needed for administering medication via the intravenous route includes the following:
- Bag of intravenous fluid
- Connective tubing (Fig. 1.28)
- Roller clamp to control the flow (Fig. 1.28)
- Needle or flexible catheter (Fig. 1.29)
- Infusion pump, if available


Reasons for Administering an Intravenous Infusion
It is relatively commonplace for patients to receive intravenous (IV) infusions when they are in hospital. Some reasons are listed below:
- To replace lost fluids: Fluids may need to be replaced because the patient has lost blood or is dehydrated.
- To administer medication: When a patient receives medication via the IV route, that medication is combined with an IV solution and usually run as a piggyback to the main line. This is discussed in more detail below, where different types of IVs are explained.
- To maintain electrolyte balance: Electrolytes such as potassium (K), for example, can be given via IV if the patient has low levels of a specific, or all, electrolytes.
- Potential to become depleted: An IV can be run at a low rate to avoid potential loss of fluids or electrolytes if they are likely to become depleted.
- Emergency situations: Emergency situations can occur during surgery or in the emergency department. In these situations, a patient may require various IV medications and fluid replacement.
- To administer blood and blood products: When blood or blood products are administered via an IV line, the line is always run secondary to an IV line of fluid in case the patient has a reaction to the blood product being given.
Different Types of Intravenous Infusions
There are different ways that IV fluids or medications can be given, and most of the subtypes of IV administration are listed below. All involve some form of IV access, which is usually through a small catheter placed into a patient’s vein.
- Primary infusion: This type of IV administration involves a bag of IV fluid connected to a primary IV line, which is attached to a small catheter in a patient’s vein. The IV line may be attached to a machine or simply use gravity, and the medication administration is measured by drip rate.
- Piggyback: In the piggyback method, a smaller secondary bag and line are attached to the primary IV infusion. This is shown in Fig. 1.30 below, where you can see the smaller bag hanging from the pole. Typically, medication is added to the secondary bag as a way of slowly administering it to the patient.
- Saline lock: In this method, a small IV line is attached to the catheter inside the patient’s vein and “locked” with a saline solution. A port on the end allows a primary infusion line to be attached if IV fluids are needed. Saline locks allow patients to be mobilized more easily because they can be detached from the longer IV line and pole. Medication can also be given through the saline lock. Another option available is a heparin lock, which allows a small dose of heparin, an anticoagulant, to be instilled in the catheter. This is less common in many hospitals but is sometimes used because it can prevent blood from clotting around the IV site and ensures that the site is not lost.
- Direct IV: In this method, shown in Fig. 1.31, medication in a syringe is attached to a port on the IV line and injected into the line so the patient receives the medication at a faster rate than they would with a piggyback.
- IV bolus: A bolus is a large amount of fluid administered in a very short time. It can also be used as a way of administering IV fluids quickly in an emergency situation.
- Keep the vein open: This is a very slow-rate infusion, often about 30 mL/hr, and is only used as a means of not losing an IV site. This is often used when there is a concern that the IV site would be lost if a saline lock was used. The abbreviation for this type of infusion is KVO.


Intravenous (IV) Solutions
Various IV solutions can be used for intravenous infusions, and many of them are used regularly in the hospital setting. The more common types are listed below, but there are others that may be used on specialty units within the hospital:
- Normal saline 0.9%: This is one of the most commonly used IV solutions and is a mixture of sodium chloride and water. It has many uses in the hospital, the most common being fluid replacement. The abbreviation for this solution is NS.
- Normal saline 0.45%: This is a less-common form of normal saline and can be considered 1/2 normal saline because the percentage of sodium chloride is half of what it would normally be.
- 2/3 dextrose and 1/3 normal saline: This solution is a mixture of dextrose (sugar) and normal saline. The common abbreviation is 2/3–1/3.
- 5% dextrose in water: This solution is a mixture of dextrose (sugar) and water. The percentage indicated can vary depending on the amount of dextrose in the solution; for example, it could be 10% or 50%. The abbreviation is D5W and may vary depending on the level of dextrose; for example, 10% dextrose in water would be D10W.
- 5% dextrose in saline: This solution is similar to D5W but is a mixture of dextrose (sugar) and saline instead of water. The amount of dextrose can vary, similar to the dextrose and water solution. The abbreviation is D5NS and can also vary depending on the level of dextrose.
- Ringer’s lactate: This solution is commonly used for fluid replacement and contains water, sodium chloride, sodium lactate, potassium chloride, and calcium chloride. The abbreviation is R/L.
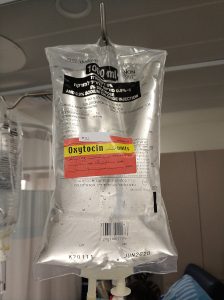
Intravenous solutions come in a variety of sizes of bags, and the intended use usually determines the size selected. Primary infusions, for example, often use a larger size, whereas piggybacks use smaller solution bags. Some available sizes include the following:
- 1,000 cc (1 litre) (Fig. 1.32)
- 500 cc
- 250 cc
- 100 cc
- 50 cc
- 25 cc
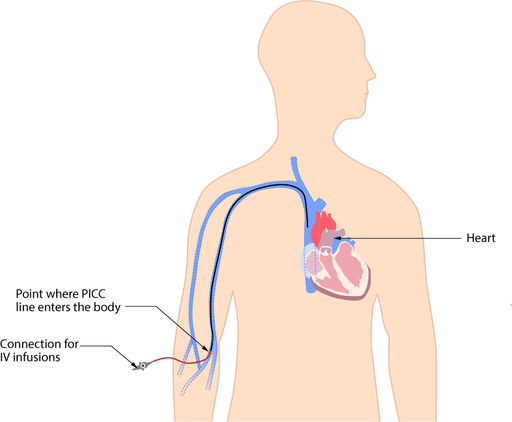
Central Lines
Central lines are often used to continuously infuse intravenous fluids and medications. As seen in Fig. 1.33, a catheter is inserted into a vein in the arm, or in some cases the neck, then the catheter is threaded through the vein and positioned near the entrance to the heart. These lines are ideal if intravenous medications are going to be administered for a long period of time and in cases when starting an intravenous line is difficult because of the patient’s vasculature.
Review
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Doyle, G. R., & McCutcheon, J. A. (2020). Clinical procedures for safer patient care. BCcampus Open Education. https://opentextbc.ca/clinicalskills/, licensed under CC BY 4.0
References
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/, licensed under CC BY 4.0
Image Credits (images are listed in order of appearance)
Subcutaneous_injection by National Institutes of Health, Public domain
Injection Sites Subcutaneous by BruceBlaus, CC BY-SA 4.0
Intramuscular (IM) Injections by Immunization Action Coalition, Public domain
Depo-Estradiol (estradiol cypionate) vials by Medgirl131, CC BY-SA 4.0
ParaldehydeAmpoule by Colin Harkness, Public domain
Intradermal injection by British Columbia Institute of Technology (BCIT), CC BY-SA 4.0
Needle-insertion-angles-1 by British Columbia Institute of Technology (BCIT), CC BY-SA 4.0
Капельница by Vlish, CC BY-SA 3.0
IV Catheters 15 by Intropin (Mark Oniffrey), CC BY-SA 4.0
Infuuszakjes by Harmid, Public domain
ICU IV 1 by Calleamanecer, CC BY-SA 3.0
Intravenous therapy oxcytocin by Eliran t, CC BY-SA 4.0
Peripherally inserted central catheter (PICC) by Glynda Rees Doyle and Jodie Anita McCutcheon, CC BY-SA 4.0