7.2 The Hematological System
The hematological system consists of blood and bone marrow, which is involved in the production of new red blood cells through a process referred to as hematopoiesis (Betts et al., 2013). Blood is technically considered a connective tissue and is made up of a mix of cellular elements within an extracellular matrix. The cellular elements include red blood cells (RBCs), white blood cells (WBCs), and cell fragments called platelets (Betts et al., 2013). The extracellular matrix, which is called plasma, makes blood unique compared to other connective tissues because it is fluid. This fluid, which is mostly water, suspends the formed elements and enables them to circulate throughout the body (Betts et al., 2013). Watch the video below as an introduction to the topic of blood and how it works within the human body.
(CrashCourse, 2015)
Functions of Blood
The primary function of blood is to deliver oxygen and nutrients and then remove wastes from body cells (Betts et al., 2013). However, blood performs other functions in the body, including defence, distribution of heat, and maintenance of homeostasis.
Transportation
Blood transports many different substances throughout the body on an ongoing basis. The nutrients from the foods that are eaten are absorbed in the digestive tract and then travel in the bloodstream directly to the liver (Betts et al., 2013). Once there, they are processed and released back into the bloodstream for delivery to body cells. In the lungs, oxygen from the air you breathe diffuses into the blood, then moves from the lungs to the heart, which pumps it to the rest of the body. Endocrine glands scattered throughout the body release their products, called hormones, into the bloodstream, which then carries them to distant target cells (Betts et al., 2013). Blood also picks up cellular wastes and byproducts, and transports them to various organs for removal. For instance, blood moves carbon dioxide to the lungs for exhalation from the body, and various waste products are transported to the kidneys and liver to be excreted in the form of urine or bile (Betts et al., 2013).
Defence
Many types of white blood cells (WBCs) protect the body from external threats, such as bacteria that can enter the bloodstream from a wound. Some types of WBCs seek out and destroy internal threats, such as cells with mutated DNA that could multiply to become cancerous, or even body cells infected with viruses (Betts et al., 2013).
When damage to the vessels results in bleeding, blood platelets and certain proteins dissolved in the plasma, the fluid portion of the blood, interact to block the ruptured areas of the blood vessels involved (Betts et al., 2013). This protects the body from further blood loss or hemorrhage.
Maintenance of Homeostasis
Blood is also involved in regulating body temperature. For example, if you were exercising on a warm day, your rising core body temperature would trigger several homeostatic mechanisms, including increased transport of blood from the core to the extremities, which are typically cooler (Betts et al., 2013). As blood passes through the vessels of the skin, heat would be released to the environment, and the blood returning to the body core would be lower in temperature. In comparison, on a cold day, blood is diverted away from the skin in order to maintain a warmer body core (Betts et al., 2013).
Blood also helps to maintain the chemical balance of the body. Proteins and other compounds in the blood act as buffers, helping to regulate the pH of body tissues. Blood also helps regulate the water content of body cells (Betts et al., 2013).
Composition of Blood
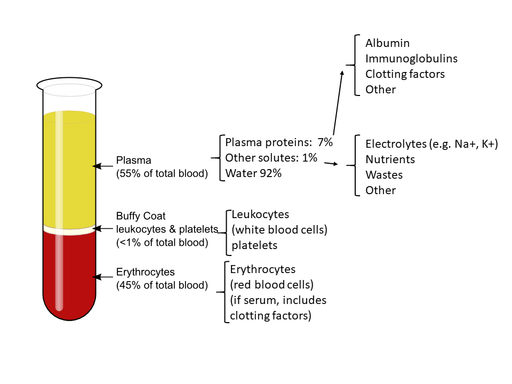
Blood is made up of three main components: hematocrit, a buffy coat, and plasma (Betts et al., 2013). Within the body, these three components are mixed together and work collaboratively to perform all the functions that blood needs to accomplish. When a blood sample is analyzed, these three components are generally separated as shown in the image below. Hematocrit consists of red blood cells (also called erythrocytes) and generally amounts to approximately 45% of a given blood sample. This percentage varies for males and females; for females, the percentage is generally between 37% to 40%, and for males, it is approximately 42% to 52%. There is also a pale, thin layer composed of the remaining formed elements of blood, which include white blood cells, platelets, and thrombocytes (Betts et al., 2013). This layer is referred to as the buffy coat because of its colour, and it normally constitutes less than 1% of a blood sample. Above the buffy coat in the test tube is the blood plasma, which is normally a pale, straw-coloured fluid and constitutes the remainder of the sample (Betts et al., 2013). Fig. 7.1 provides a breakdown of the blood components found in the body and in a given sample.
Characteristics of Blood
Often when someone thinks about blood, the first characteristic that comes to mind is its colour. Blood that has just taken up oxygen in the lungs is bright red, and blood that has released oxygen to the tissues is a more dusky red. This is because the hemoglobin in the blood is a pigment that changes colour depending on the degree of oxygen saturation (Betts et al., 2013).
Blood is viscous and somewhat sticky to the touch. Its viscosity is approximately five times greater than that of water. Viscosity is a measure of a fluid’s thickness or resistance to flow and is influenced by the presence of the plasma proteins and formed elements within the blood (Betts et al., 2013). The viscosity of blood has a dramatic impact on blood pressure and flow. Consider the difference in flow between water and honey. The more viscous honey has a greater resistance to flow than the less viscous water (Betts et al., 2013).
The normal temperature of blood is slightly higher than normal body temperature and is usually about 38°C (or 100.4°F), compared to 37°C (or 98.6°F) for an internal body temperature reading (Betts et al., 2013). Although the surface of blood vessels is relatively smooth as blood flows through them, the blood experiences some friction and resistance, especially as vessels age and lose their elasticity, which then produces heat (Betts et al., 2013).
Blood Clots and Other Key Terms
Blood clots can form in the body in response to damage and help the body control bleeding both internally and externally. Thrombus is the term for a blood clot that forms in a vein or artery. Thrombi (the plural form of “thrombus”) are commonly caused by damage to a blood vessel, which then activates the clotting process within that vessel. Often the terms “blood clot” and “thrombus” are used interchangeably, with the main difference being the location of origin. A blood clot, or thrombus, is generally made up of a collection of platelets, red blood cells, and white blood cells that are kept together by a substance called fibrin.
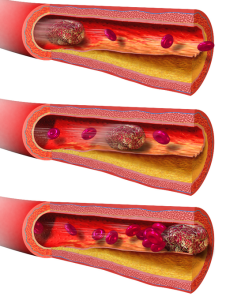
An embolus is a thrombus, or blood clot, that breaks off and moves through the blood vessels until it reaches a vessel that is so small it becomes stuck. When this happens, blood flow is stopped beyond that area. Fig. 7.2 shows how an embolus may travel through a vessel until it ultimately becomes trapped and blocks blood from travelling beyond that site.
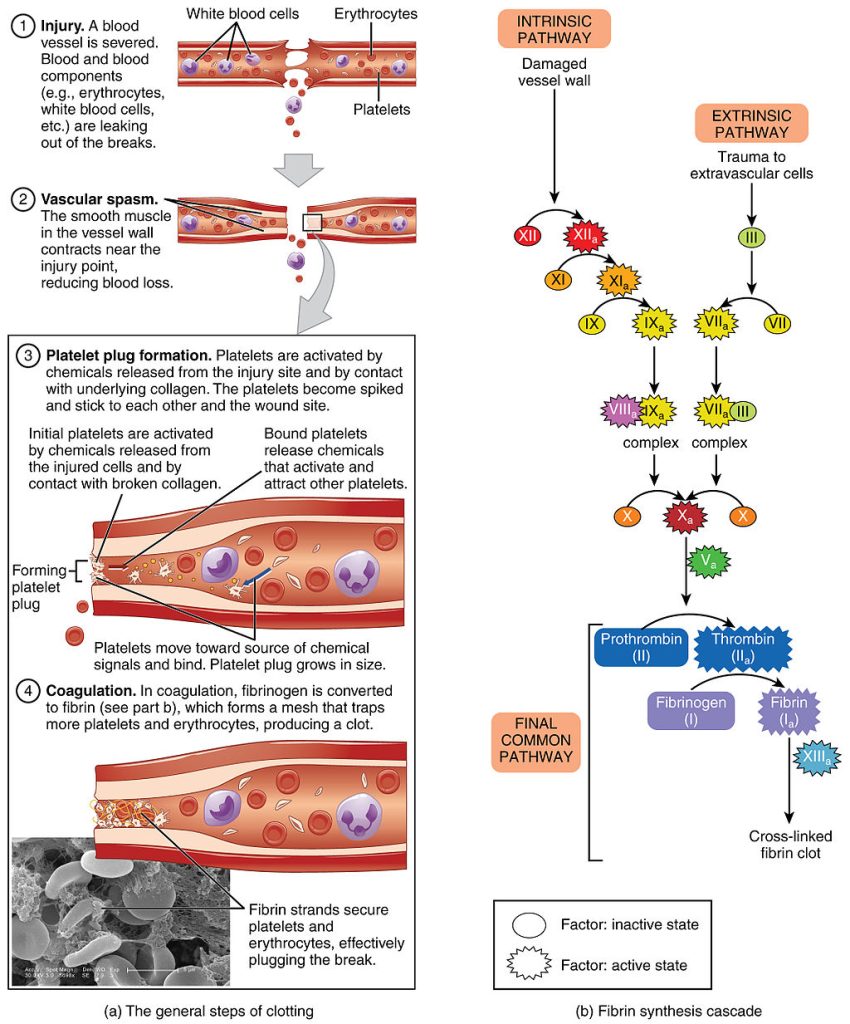
The formation of a thrombus, or blood clot, can be called coagulation, which is the process of a liquid, in this case blood, changing to a solid or semi-solid state. The process is sometimes seen as a cascade because one event prompts the next in this complex and sequential process.
Coagulation Cascade
The coagulation cascade is a complex process the body goes through in order for a blood clot to form. This process can begin through either intrinsic or extrinsic pathways, which simply means it can begin through an injury (extrinsic) or as a result of internal damage to a cell wall (intrinsic) (Betts et al., 2013). Once it begins, the cascade involves the activation of a series of clotting factors (Factors I–VIII) that are required for a clot to ultimately be formed. Clotting factors are proteins involved in the clotting process and are secreted mainly by the liver. Vitamin K, biotin, folate, and calcium are heavily involved and are required by the liver to produce these clotting factors (Betts et al., 2013). Fig. 7.3 below provides a very detailed illustration of the process the body goes through and the factors that play a role in the process.
Another key concept to understand is the role ofanticoagulants, which are substances that oppose coagulation. Your body naturally has several circulating plasma anticoagulants that limit the coagulation process at the region of injury and restore a normal, clot-free condition of blood. Anticoagulant medications work in various ways; however, they often involve inhibiting the clotting factors in the blood or inhibiting the formation of clotting factors in the liver, which requires vitamin K. They can also prevent platelets from adhering to the site of an injury and from clumping together to begin to form a clot. Finally, anticoagulants can also decrease the viscosity of the blood and increase red blood cell flexibility so as to increase blood flow.
Another class of drugs is known as thrombolytic agents, and these are used, not to prevent a clot, but rather to dissolve an unwanted clot. Thrombolytic agents are given to a patient within a few hours after a cerebrovascular accident (stroke) or myocardial infarction (heart attack) to dissolve the clot and improve the patient’s prognosis.
Did you know?
According to the Institute for Safe Medication Practices (ISMP) 2016 Annual Report, there is a high risk of acute injuries for patients taking anticoagulants outside the hospital setting. Anticoagulants are commonly used by the geriatric population to reduce the risk of ischemic stroke. An estimated 3.8 million people took oral anticoagulants in 2016 (Institute for Safe Medication Practices, 2017). Centers for Disease Control data show that adverse effects of oral anticoagulants account for more emergency department visits than any other class of drugs. Adverse effects range from gastrointestinal bleeding to cerebral hemorrhages and resulted in over 3,000 deaths in 2016 (Institute for Safe Medication Practices, 2017).
Diagnostic Lab Tests
It is always important to evaluate a patient’s response to a medication, and this is especially true with anticoagulants. Often, laboratory tests are ordered to ensure that the patient’s blood is clotting as it should. If it is clotting too much, then the patient is at risk for a blood clot, or embolus, and if it is not clotting enough, then the patient is at risk of hemorrhage. Many anticoagulant medications also require regular dose adjustments to produce the desired effect. For example, intravenous heparin is often administered according to a protocol that requires dose adjustment based on partial thromboplastin time (PTT) lab results to achieve a therapeutic range and avoid overdosing, which can result in a life-threatening hemorrhage.
Many patients outside the hospital setting may take anticoagulant medications such as warfarin to prevent blood clots. Warfarin requires regular laboratory monitoring and dose adjustments based on prothrombin time (PT) and international normalized ratio (INR) lab results. All of these lab tests involve some manner of assessing the effectiveness of clotting factors in a sample of serum.
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/, licensed under CC BY 4.0
References
Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Anatomy and physiology. OpenStax. https://openstax.org/details/books/anatomy-and-physiology, licensed under CC BY 4.0
CrashCourse. (2015, August 3 ). Blood, part 1 – True blood: Crash Course anatomy & physiology #29 [Video]. YouTube. https://www.youtube.com/watch?v=HQWlcSp9Sls
Institute for Safe Medication Practices (ISMP). (2017, July 27). QuarterWatch™ (2016 Annual Report) part II: Oral anticoagulants—The nation’s top risk of acute injury from drugs. https://www.ismp.org/resources/quarterwatchtm-2016-annual-report-part-ii-oral-anticoagulants-nations-top-risk-acute
Image Credits (images are listed in order of appearance)
Components_of_blood by Alan Sved, CC BY-SA 4.0
Blausen_0089_BloodClot_Motion by BruceBlaus, CC BY 3.0
1909_Blood_Clotting by OpenStax College, CC BY 3.0
the formation of blood cellular components
the steady state of body systems that living organisms maintain
the percentage of red blood cells in blood
the oxygen-carrying compound in erythrocytes (red blood cells)
having a thick, sticky consistency between solid and liquid
gel-like clumps of blood
a blood clot that forms in a vein or artery
the formation of a thrombus or blood clot
a substance that opposes or prevents coagulation
medications used to dissolve a major clot quickly
a blood test that looks at how long it takes for blood to clot; abbreviated as PTT
a test that evaluates blood clotting
a test that measures the time required for blood to clot; abbreviated as INR