11.2 Physiology of Pain
Before learning about the medications that are used to treat a patient’s pain, it is important to review the physiology of pain, the types of pain, the means of assessing pain, and the reasons for administering analgesics.
Physiology of Pain
Pain occurs when there is tissue damage in the body. Tissue damage activates the pain receptors of the peripheral nerves. Nociceptors, which are the nerve endings that respond to painful stimuli, are located in arterial walls, joint surfaces, muscle fascia, periosteum, skin, and soft tissue. The cause of tissue damage may be physical, such as heat or pressure, or chemical, which results from pain-producing substances being released into the extracellular fluid surrounding the nerve fibres. These pain-producing substances activate pain receptors, increase the sensitivity of pain receptors, or possibly stimulate the release of inflammatory substances, such as prostaglandins.
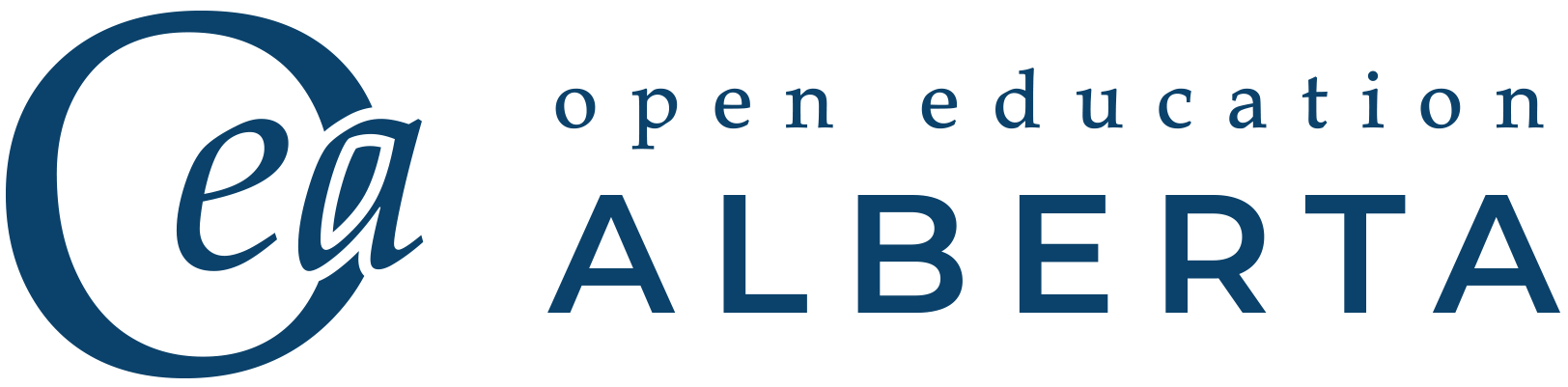
For a person to feel pain, the signal from the nociceptors in peripheral tissues must be transmitted to the spinal cord and then to the hypothalamus and cerebral cortex of the brain. The signal is transmitted to the brain by two types of nerve cells—A-delta and C fibres. The dorsal horn of the spinal cord is the relay station for information from these fibres. In the brain, the thalamus is the relay station for incoming sensory stimuli, including pain. From the thalamus, the pain messages are relayed to the cerebral cortex, where they are perceived. This complex pathway can be seen in Fig. 11.1 below.
Endogenous Analgesia
The central nervous system (CNS) actually has its own endogenous analgesia system for relieving pain. The CNS suppresses pain signals from peripheral nerves. Opioid peptides interact with opioid receptors to inhibit the perception and transmission of pain signals. These opioid peptides are endorphins, enkephalins, and dynorphins.
See the video below for more information about how the body perceives pain and an overview of how pain relievers work within the body. This will introduce you to some of the discussion that you will find in this chapter.
(TED-Ed, 2012)
Types of Pain
Acute Pain
Acute pain comes on suddenly and is caused by something specific, such as a trauma. It is sharp in quality and usually does not last longer than a month. It goes away when there is no longer an underlying cause for the pain, either because the body has corrected the issue or medical treatment has relieved the causative factor.
Causes of acute pain include the following:
- Surgery
- Broken bones
- Dental work
- Burns or cuts
- Labour and childbirth
Chronic Pain
Chronic pain is pain that is ongoing and usually lasts longer than a couple of months. This type of pain can continue even after the injury or illness that caused it has healed or gone away. Pain signals remain active in the nervous system for weeks, months, or years. Some people suffer chronic pain even when there is no past injury or apparent body damage.
Chronic pain is linked to some health conditions:
- Arthritis
- Cancer
- Nerve pain
- Back pain
- Fibromyalgia pain
People who have chronic pain can have physical effects that are stressful on the body. These include tense muscles, limited ability to move around, lack of energy, and appetite changes. It is common to also have emotional effects of chronic pain, which can include depression, anger, anxiety, and fear of reinjury.
Pain Assessment
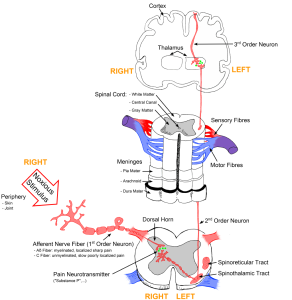
Analgesic medications are given to alleviate pain. However, pain can be subjective and vary from person to person, so it is important to have ways of measuring someone’s level of pain. This is accomplished by using different forms of a pain scale. Pain can be assessed according to a number of mnemonics (memory aids), such as PQRST (Provoking factors, Quality, Region/Radiation, Severity, Time) or simply measured according to a scale from 1 to 10, with 10 being the worst pain the patient has ever felt and 1 being no pain at all (Fig. 11.3). Visual pain scales have been developed as tools for communicating about pain with children through to patients at the end of life (Fig. 11.2). Visual pain scales are also helpful if the healthcare provider and the patient speak different languages or there are other communication issues.

The Ideal Analgesic
Throughout this chapter, we will discuss many common analgesics that can be used to relieve mild, severe, chronic, and acute pain. Pain is a phenomenon that unfortunately is seen on a daily basis within the community and throughout health care. This makes an “ideal analgesic” something that is greatly sought after and needed. In order for an analgesic to be “ideal,” it would have to have certain qualities, including maximum pain relief, no side effects, and no possibility for addiction. Sadly, this ideal analgesic does not exist, as none of the medications that will be discussed have all of these qualities.
Types of Analgesics
Analgesics used to treat pain are categorized as non-narcotic (non-opioid), narcotic (opioid), and adjuvant medications. Non-narcotic medications include acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs). There are several types of narcotics, and because of the possibility of abuse and addiction, they are all highly controlled. Adjuvants are defined as medications with a primary use other than pain relief, though they have analgesic properties in some painful conditions. This group includes numerous medications in various classes such as gabapentin (an anticonvulsant), amitriptyline (a tricyclic antidepressant), and certain muscle relaxants. We will discuss all these types of analgesics later in the chapter.
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Ernstmeyer, K., & Christman, E. (Eds.). (2020). Nursing pharmacology. Chippewa Valley Technical College. https://wtcs.pressbooks.pub/pharmacology/, licensed under CC BY 4.0
References
TED-Ed. (2012, June 26). How do pain relievers work? – George Zaidan [Video]. YouTube. https://youtu.be/9mcuIc5O-DE
Image Credits (images are listed in order of appearance)
Sketch colored final by Bettina Guebeli, CC BY-SA 4.0
Children’s pain scale by Robert Weis, CC BY-SA 4.0
Pain scale with words by MissLunaRose12, CC BY-SA 4.0
nerve endings that respond to painful stimuli
a group of lipids that are made at sites of tissue damage or infection
originating from within an organism
analgesic medications that are often available without a prescription and are used to treat mild to moderate pain
analgesic medications that are available with a prescription, are highly regulated, and are used to treat moderate to severe pain
medications with a primary use other than pain relief that have analgesic properties in some painful conditions