Communication
Proxemics
Open Resources for Nursing (Open RN)
Personal Space
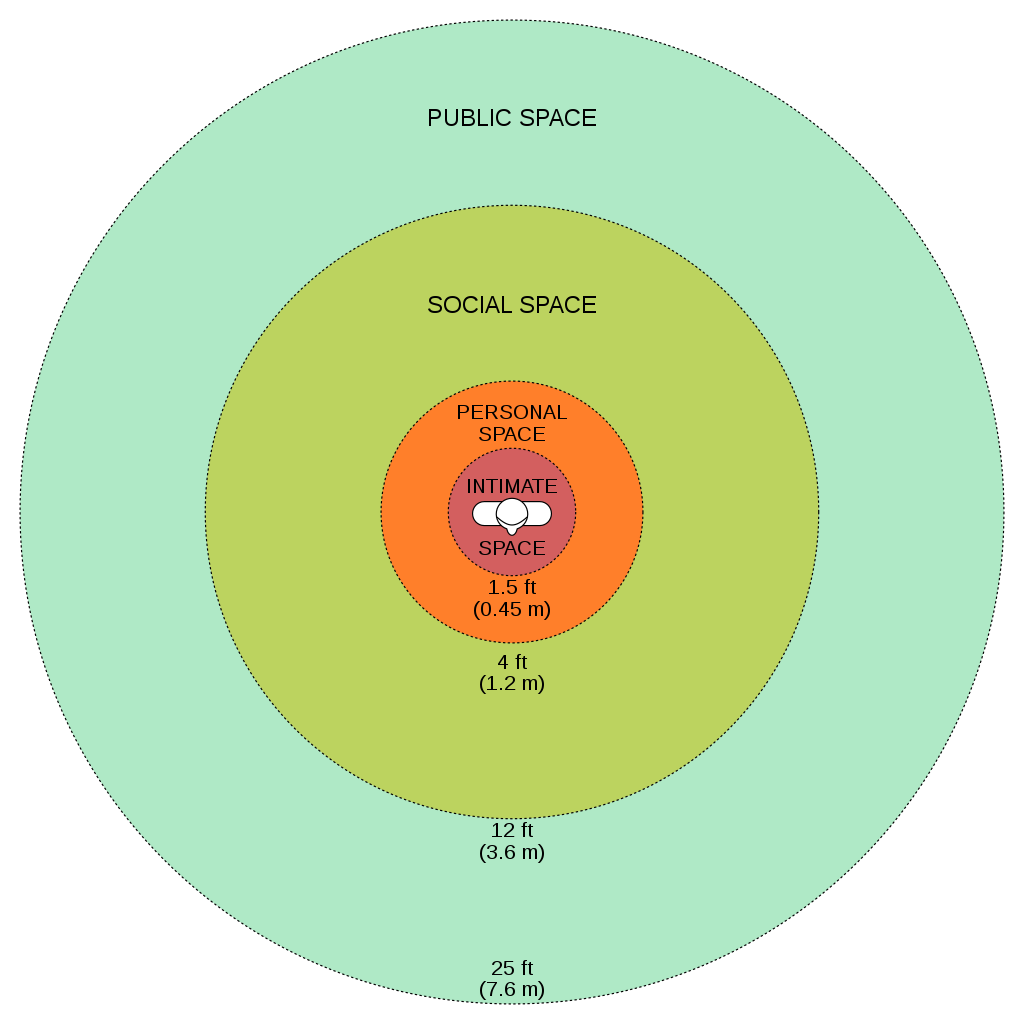
While being aware of verbal and nonverbal messages and communicating assertively, it is also important to be aware of others’ personal space. Proxemics is the study of personal space and provides guidelines for professional communication. The public zone is over 10 feet of distance between people and generally avoids physical contact. The social zone is four to 10 feet of distance between people. It is used during social interactions and business settings. The personal zone is 18 inches to four feet of space and is generally reserved for friends and family. Less than 18 inches is reserved for close relationships but may be invaded when in crowds or playing sports.[1] Nurses usually communicate within the social zone to maintain professional boundaries. However, when assessing patients and performing procedures, nurses often move into a patient’s personal zone. Nurses must be aware of patients’ feelings of psychological discomfort that can occur when invading this zone. Additionally, cultural considerations may impact the appropriateness of personal space when providing patient care. See Figure 2.6 for example of personal space zones.[2]
Overcoming Common Barriers to Communication
It is important for you to reflect on personal factors that influence your ability to communicate effectively. There are many factors that can cause the message you are trying to communicate to become distorted and not perceived by the receiver in the way you intended. It is important to seek feedback that your message is clearly understood. Nurses must be aware of these potential barriers and try to reduce their impact by continually seeking feedback and checking understanding.[3]
Common barriers to communication in health care and strategies to overcome them are described in the following box.[4]
Common Barriers to Communication in Health Care
- Jargon: Avoid using medical terminology, complicated, or unfamiliar words. When communicating with patients, explain information in plain language that is easy to understand by those without a medical or nursing background.
- Lack of attention: Nurses are typically very busy with several tasks to complete for multiple patients. It is easy to become focused on the tasks instead of the patient. When entering a patient’s room, it is helpful to pause, take a deep breath, and mindfully focus on the patient in front of you to give them your full attention. Patients should feel as if they are the center of your attention when you are with them, no matter how many other things you have going on.
- Noise and other distractions: Health care environments can be very noisy with people talking in the room or hallway, the TV blaring, alarms beeping, and pages occurring overhead. Create a calm, quiet environment when communicating with patients by closing doors to the hallway, reducing the volume of the TV, or moving to a quieter area, if possible.
- Light: A room that is too dark or too light can create communication barriers. Ensure the lighting is appropriate according to the patient’s preference.
- Hearing and speech problems: If your patient has hearing or speech problems, implement strategies to enhance communication. See the “Adapting Your Communication” section below for strategies to address hearing and speech problems.
- Language differences: If English is not your patient’s primary language, it is important to seek a medical interpreter and to also provide written handouts in the patient’s preferred language when possible. Most agencies have access to an interpreter service available by phone if they are not available on-site.
- Differences in cultural beliefs: The norms of social interaction vary greatly in different cultures, as well as the ways that emotions are expressed. For example, the concept of personal space varies among cultures, and some patients are stoic about pain whereas others are more verbally expressive. Read more about caring for diverse patients in the “Diversity” chapter.
- Psychological barriers: Psychological states of the sender and the receiver affect how the message is sent, received, and perceived. For example, if nurses are feeling stressed and overwhelmed with required tasks, the nonverbal communication associated with their messages such as lack of eye contact, a hurried pace, or a short tone can affect how the patient perceives the message. If a patient is feeling stressed, they may not be able to “hear” the message or they may perceive it differently than it was intended. It is important to be aware of signs of the stress response in ourselves and our patients and implement appropriate strategies to manage the stress response. See the box below for more information about strategies to manage the stress response.
- Physiological barriers: It is important to be aware of patients’ potential physiological barriers when communicating. For example, if a patient is in pain, they are less likely to hear and remember what was said, so pain relief should be provided as needed before providing patient education. However, it is also important to remember that sedatives and certain types of pain medications often impair the patient’s ability to receive and perceive messages so health care documents cannot be signed by a patient after receiving these types of medications.
- Physical barriers for nonverbal communication: Providing information via e-mail or text is often less effective than face-to-face communication. The inability to view the nonverbal communication associated with a message such as tone of voice, facial expressions, and general body language often causes misinterpretation of the message by the receiver. When possible, it is best to deliver important information to others using face-to-face communication so that nonverbal communication is included with the message.
- Differences in perception and viewpoints: Everyone has their own beliefs and perspectives and wants to feel “heard.” When patients feel their beliefs or perspectives are not valued, they often become disengaged from the conversation or the plan of care. Nurses should provide health care information in a nonjudgmental manner, even if the patient’s perspectives, viewpoints, and beliefs are different from their own.
Managing the Stress Response[5]
The stress response is a common psychological barrier to effective communication. It can affect the message sent by the sender or how it is received by the receiver. The stress response is a common reaction to life events, such as a nurse feeling stressed by being overwhelmed with tasks to complete for multiple patients, or a patient feeling stressed when admitted to a hospital or receiving a new diagnosis. Symptoms of the stress response include irritability, sweaty palms, a racing heart, difficulty concentrating, and impaired sleep. It is important to recognize symptoms of the stress response in ourselves and our patients and use strategies to manage the stress response when communicating. Strategies to manage the stress response are as follows:
- Use relaxation breathing. Become aware of your breathing. Take a deep breath in your nose and blow it out through your mouth. Repeat this process at least three times in succession and then as often as needed throughout the day.
- Make healthy diet choices. Avoid caffeine, nicotine, and junk food because these items can increase feelings of anxiety or being on edge.
- Make time for exercise. Exercise stimulates the release of natural endorphins that reduce the body’s stress response and also helps to improve sleep.
- Get enough sleep. Set aside at least 30 minutes before going to bed to wind down from the busyness of the day. Avoid using electronic devices like cell phones before bedtime because the backlight can affect sleep.
- Use progressive relaxation. There are several types of relaxation techniques that focus on reducing muscle tension and using mental imagery to induce calmness. Progressive relaxation generally includes the following steps:
- Start by lying down somewhere comfortable and firm, like a rug or mat on the floor. Get yourself comfortable.
- Relax and try to let your mind go blank. Breathe slowly, deeply, and comfortably, while gradually and consciously relaxing all your muscles, one by one.
- Work around the body one main muscle area at a time, breathing deeply, calmly, and evenly. For each muscle group, clench the muscles tightly and hold for a few seconds, and then relax them completely. Repeat the process, noticing how it feels. Do this for each of your feet, calves, thighs, buttocks, stomach, arms, hands, shoulders, and face.
Media Attributions
- 1024px-Personal_Space.svg
- Psychology Today. (n.d.) Proxemics. https://www.psychologytoday.com/us/basics/proxemics ↵
- “Personal Space.svg” by WebHamster is licensed under CC BY-SA 3.0 ↵
- SkillsYouNeed. (n.d.). Barriers to effective communication. https://www.skillsyouneed.com/ips/barriers-communication.html ↵
- SkillsYouNeed. (n.d.). Barriers to effective communication. https://www.skillsyouneed.com/ips/barriers-communication.html ↵
- American Psychological Association. (2019). Healthy Ways to Handle Life's Stressors. https://www.apa.org/topics/stress/tips ↵