53 Glucose-6-phosphate Dehydrogenase (G6PD) Deficiency
Michelle To and Valentin Villatoro
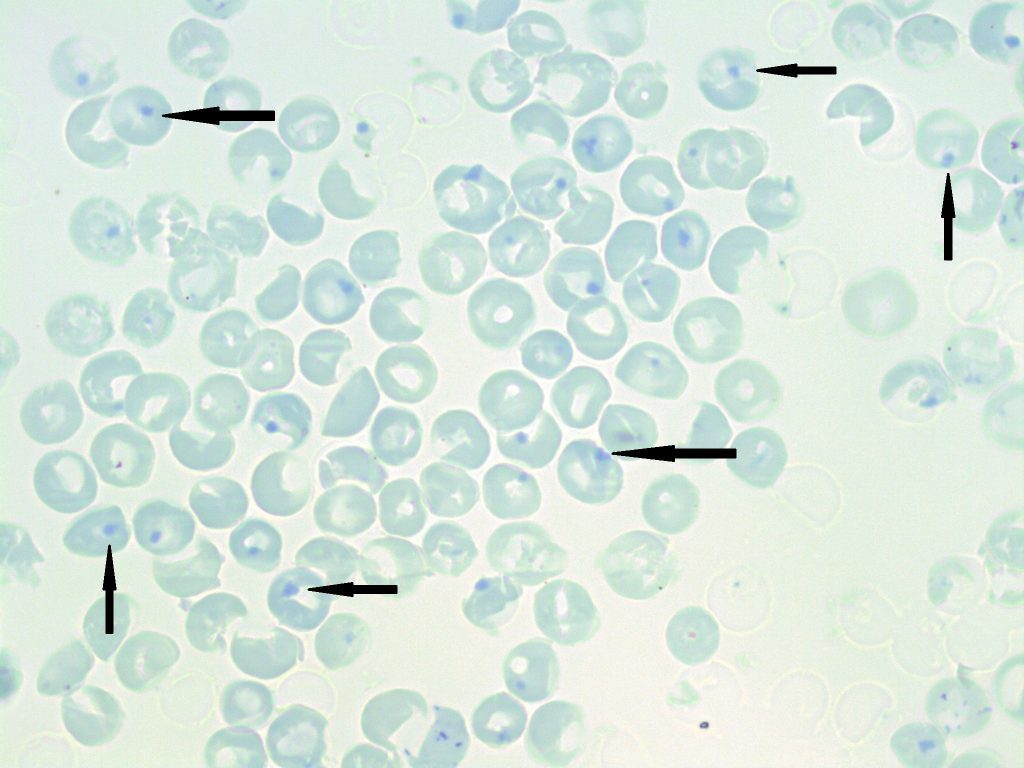
- A peripheral blood smear stained with a supravital stain demonstrating numerous heinz bodies (indicated by arrows). 100x oil immersion. From MLS Collection, University of Alberta, https://doi.org/10.7939/R35718396
Normal G6PD Function: Hexose Monophosphate (HMP) Shunt and Oxidative Damage1,2
The HMP Shunt describes the glycolytic pathway where glucose is transferred to and catabolized in the cell to produce ATP and maintain sustainable amounts of reduced glutathione (GSH). GSH acts to protect the red blood cell from oxidative damage by reducing oxidative molecules (Peroxides and free oxygen radicals) and becoming oxidized itself.
In the HMP shunt, NADPH is generated by G6PD from NADP which than acts to regenerate reduced glutathione from its oxidized state to allow continued protection from oxidative damage. A lack of G6PD results in increased red blood cell destruction.
G6PD activity is highest in younger cells (i.e. reticulocytes) compared to that of older and more mature red blood cells.1
Mutation:2
G6PD gene mutation results in decreased G6PD levels.
Inheritance:1
X-linked
Complications:1,2
Acute hemolytic Anemia
Neonatal Hyperbilirubinemia
Chronic Nonspherocytic Hemolytic Anemia
Causes of Hemolytic Episodes:1,2
Exposure to oxidative agents:
-Drugs (e.g. antimalarials, sulfonamides)
-Infections
-Fava Beans (Favism)
Notes:
G6PD deficiency is commonly associated with bite and blister cells. Oxidized hemoglobins become denatured and form heinz bodies within the red blood cells. These heinz bodies can be removed by splenic macrophages through a “pitting” mechanism, which results in the formation of bite and blister cells.1
It has been suggested that G6PD deficiency acts as a protective mechanism from malaria as the prevalence of G6PD deficiency coincides with that of malaria.1
Laboratory Results for G6PD Deficiency:1
|
CBC: WBC: Increased PLT: Normal Hb: Decreased MCHC: Increased RETIC: Increased |
PBS: Bite and Blister Cells Polychromasia Occasional spherocytes Heinz bodies (Supravital staining) |
Other Tests: Dye Reduction Test: No colour change G6PD Assay: Decreased activity DAT: Negative
Hemolysis Markers: Indirect Bilirubin: Increased LDH: Increased Haptoglobin: Decreased Hemoglobinemia Hemoglobinuria |
References:
1. Lake M, Bessmer D. Hemolytic anemia: enzyme deficiencies. In: Clinical laboratory hematology. 3rd ed. New Jersey: Pearson; 2015. p. 334-47.
2. Keohane EM. Intrinsic defects leading to increased erythrocyte destruction. In: Rodak’s hematology clinical applications and principles. 5th ed. St. Louis, Missouri: Saunders; 2015. p. 367–93.