8.4 Diagnostic Imaging: Nuclear Medicine, Ultrasound, and MRI
This section will discuss other common forms of diagnostic imaging. The physician’s choice of which type of imagining will be used for a particular patient is determined by the patient’s condition, history, need, and the availability of testing. For example, not all hospitals will be able to offer an MRI or nuclear medicine. Three of the more common types of imagining, other than radiology, are discussed in detail below, and examples of scans are provided.
Nuclear Medicine

Nuclear medicine tests and procedures have one main commonality—the use of a radioactive substance to enhance the scan. The patient is injected with a radioactive pharmaceutical agent and becomes the source of the radiation required to produce the nuclear medicine images. The pharmacologic agent concentrates in different organs and tissues based on the patient’s physiology and the components of the agent. Fig. 8.30 is an image of a nuclear medicine scanner in a hospital. After the patient is injected with the radioactive pharmaceutical agent, they lie on the machine’s table in a supine position while the machine detects the emitted radiation.
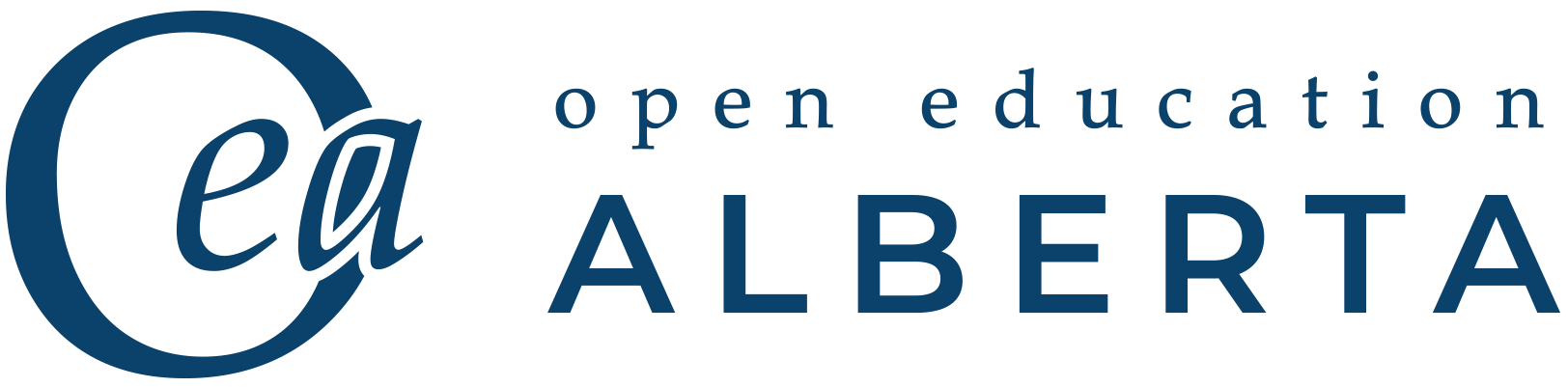
A number of areas of the body can be assessed using radioactive substances to enhance the images; for example, a thyroid scan, shown in Fig. 8.31, is a common procedure. For bone scans, the radioactive substance technetium-99m is used because it contains diphosphonate, which interacts physiologically with living bone. As a result, when the scan is done, radioactivity is shown as arising from the patient’s bones. Fig. 8.32 shows an example of a pediatric bone scan. Similarly, a renal scan shows the kidneys, ureters, and bladder as the pharmacologic agent is metabolized and concentrated in these tissues. Lung scans can be done to provid a better understand of any pathology that may be present in a patient’s respiratory system.

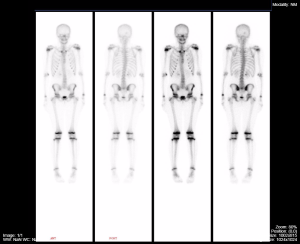
A multigated acquisition scan (MUGA) is a diagnostic test used to evaluate the pumping action of the ventricles of the heart (Cleveland Clinic, 2022). Similar to the tests mentioned above, a small amount of radioactive tracer is injected into a patient’s vein, then a technician uses a camera to detect the radiation that is released by the tracer. This results in computer-generated, movie-like images of the beating heart. This test results in a very detailed record of the heart’s pumping function (Cleveland Clinic, 2022). Fig. 8.33 is an example of a MUGA scan.

A positron emission tomography (PET) scan is an imaging test that is used to reveal the metabolic or biochemical function of tissues and organs (Betts et al., 2013). The PET scanner (Fig. 8.34) also uses a radioactive substance to show both normal and anomalous metabolic activity. PET scans are often used to diagnose conditions such as heart disease, the spread of cancer, certain forms of infection, brain abnormalities, bone disease, and thyroid disease (Betts et al., 2013).
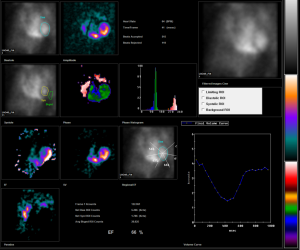
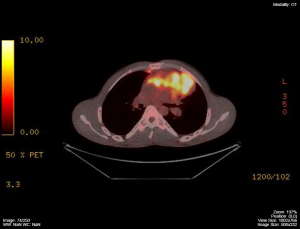
Positron emission tomography – Computed tomography (PET-CT) is a combination of PET and CT scans. It provides a simultaneous CT scan while the PET scan is being completed (Betts et al., 2013). The appeal of this approach is that it is possible to overlay (fuse) one image with the other to match the activity level of positron emission with the anatomy seen on the CT. Fig. 8.35 and Fig. 8.36 show different forms of PET-CTs, though both are examples of patients with multiple lymphomas.
Ultrasound
A majority of the general population has likely had an ultrasound or knows someone who has. Often we think of pregnancy when discussing ultrasounds; however, this type of imaging can be used for many other physiological functions as well. For diagnostic purposes, ultrasounds are used for most parts of the human body. They can assist with studying heart function, blood flow in the neck or extremities, certain conditions such as gallbladder disease, and fetal growth and development.
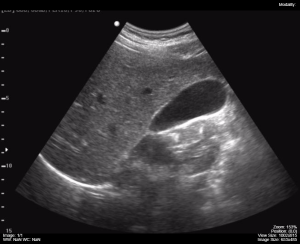
Ultrasounds rely on high-frequency, inaudible sound arising from a hand-held transducer, or probe, to create images. The transducer emits ultrasounds roughly 5% of the time, then listens for the returning echoes 95% of the time. An acoustic gel is used to help facilitate ultrasound transmission when it is applied to the probe and to the patient’s skin to minimize the air-gap between the probe and the skin. The main disadvantages of ultrasound imaging are that the image quality is heavily operator-dependent and that ultrasounds are unable to penetrate bone and gas. Fig 8.37 shows an example of a technician preforming an ultrasound on a patient, and Fig. 8.38 is an example of a gallbladder ultrasound.

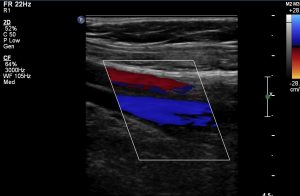
Doppler ultrasound can analyze flowing fluids, the presence of blood clots, and determine whether there is a frequency shift over the length of a structure. Colour can also be applied to the image to represent the direction of blood flow. Blood flowing toward the transducer is orange-red, and blood flowing away is blue. The varying colours in Doppler ultrasounds can be seen in Fig. 8.39 and Fig. 8.40.

An echocardiogram is a type of sonogram that may be ordered if a vascular disorder is suspected. It is a combination of an ultrasound that monitors blood flow and electrodes that monitor heart rhythm. Abnormal heart sounds can indicate a valve or septal disorder, and an echocardiogram can assist with diagnosis.
Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) is a noninvasive medical imaging technique based on nuclear magnetic resonance discovered in the 1930s; matter exposed to magnetic fields and radio waves emits radio signals that can be converted to images (Betts et al., 2013). In 1970, a physician named Raymond Damadian noticed that malignant tissue gave off different signals than normal body tissue. He applied for a patent for the first MRI scanning device, which was in use clinically by the early 1980s (Betts et al., 2013). The early MRI scanners were crude and basic, but advances in digital computing and electronics led to advancements in MRIs, which resulted in them becoming the most precise technique for medical imaging, especially to discover tumours. Fig. 8.41 shows an MRI machine, and Fig. 8.42 is a detailed MRI scan of the lumbar spine, which demonstrates the detail available with this form of imaging. MRI also has the significant advantage of not exposing patients to radiation. The drawbacks of MRI scans include their much higher cost and patient discomfort with the procedure (Betts et al., 2013).


The MRI scanner subjects the patient to such powerful electromagnets that the scan room must be shielded (Betts et al., 2013). The patient must also be enclosed in a metal tube-like device for the duration of the scan, which can sometimes be as long as 90 minutes, and can be uncomfortable and impractical for very ill patients (Betts et al., 2013). The device is also very noisy so that, even with earplugs, patients can become anxious. This problem has been partially overcome with the development of “open” MRI scanning, which does not require the patient to be entirely enclosed in the metal tube. Patients with iron-containing metallic implants, such as internal sutures and prosthetics, cannot undergo MRI scanning because it can dislodge these implants (Betts et al., 2013).
Functional MRIs (fMRIs), which can detect the concentration of blood flow in certain parts of the body, are increasingly being used to study the activity in parts of the brain during various body activities. This technology helps us learn more about the locations of different brain functions and about brain abnormalities.
Exercise
Attribution
Unless otherwise indicated, material on this page has been adapted from the following resource:
Burbridge, B. (2017). Undergraduate diagnostic imaging fundamentals. University of Saskatchewan, Distance Education Unit. https://openpress.usask.ca/undergradimaging/ licensed under CC BY-NC-SA 4.0
References
Betts, J. G., Young, K. A., Wise, J. A., Johnson, E., Poe, B., Kruse, D. H., Korol, O., Johnson, J. E., Womble, M., & DeSaix, P. (2013). Anatomy and physiology. OpenStax. https://openstax.org/details/books/anatomy-and-physiology licensed under CC BY 4.0 1
Cleveland Clinic. (2022). Multigated acquisition scan (MUGA). https://my.clevelandclinic.org/health/diagnostics/17247-multigated-acquisition-scan-muga#:~:text=What%20is%20a%20MUGA%20scan,is%20injected%20into%20a%20vein
Image Credits (images are listed in order of appearance)
Nuclear medicine scanner 1 by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Thyroid scan by Myohan, CC BY 3.0
Normal pediatric nuclear medicine bone scan by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Normal MUGA scan 1 by Jmarchn, CC BY-SA 3.0
Helical CT Scanner 1 by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
PET, whole body image, for a patient with lymphoma by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
PET/CT – Fused image, PET image superimposed on the of the axial chest CT for a patient with lymphoma by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Ultrasound machine by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Gallbladder by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Colour Doppler of the neck by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Carotid Doppler ultrasound 1 by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Magnetic Resonance Imaging Machine by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Lumbar Spine MRI T1 Sequence – Dark Cerebrospinal Fluid, Sagittal Plane by Dr. Brent Burbridge MD, CC BY-NC-SA 4.0
Growing in an uncontrolled or invasive way; typically refers to cancer that has spread to nearby organs or tissues